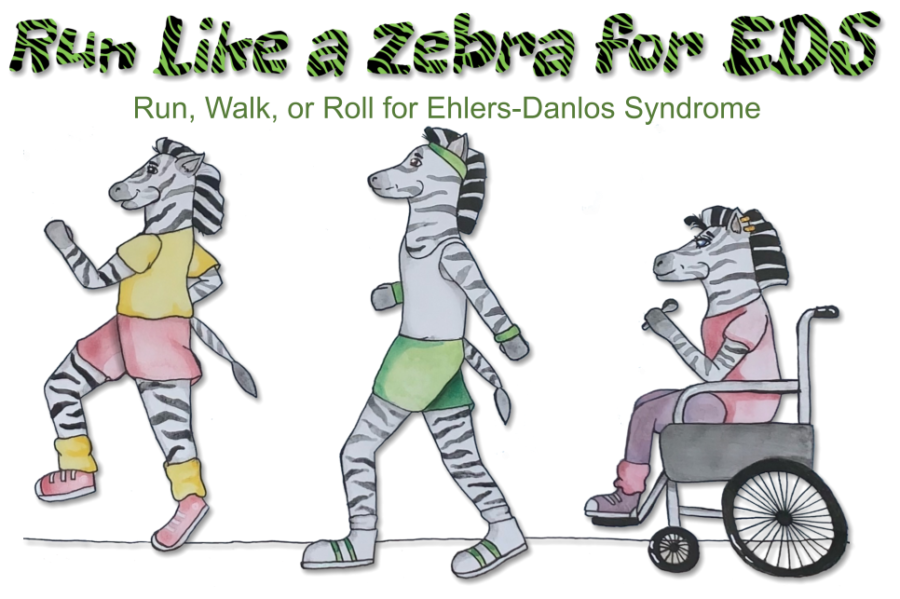
Dysautonomia Patient Guide
Version: September 2023
Written by Karina Sturm
Reviewed by Dr. med. Natalie Börsch
Copyright: Chronic Pain Partners/EDS Awareness
Disclaimer: This is no medical advice, nor is this patient guide an exclusive list of any sort. Please consult with your healthcare provider for all your medical concerns.
What is Dysautonomia?
Dysautonomia is an umbrella term that describes disorders of the autonomic (vegetative) nervous system [1]. The autonomic nervous system controls all involuntary processes in the body, such as digestion or heart rate. We can distinguish between primary and secondary dysautonomias [2]. Primary dysautonomias occur without an underlying cause, while secondary dysautonomias result from an underlying condition. Disorders of the autonomic nervous system can affect any area of the body and can severely impact the affected person.
The Nervous System
Central vs. Peripheral [3, 4]
Our nervous system is responsible for perceiving, processing, and transmitting information.
It consists of the Central Nervous System (CNS), formed by the brain and spinal cord, and the Peripheral Nervous System (PNS), which includes the nerve fibers that carry information between the periphery and the brain.
All nerves outside the brain and spinal cord belong to the Peripheral Nervous System. The Peripheral Nervous System can be further divided into the autonomic (vegetative) and somatic nervous systems.
The somatic nervous system controls all voluntary functions of the body, such as skeletal muscles.
Classification of the autonomic nervous system [5]:
- Sympathetic Nervous System: The sympathetic nervous system triggers the body’s “fight or flight” response. It increases heart rate and blood pressure, accelerates metabolism, and influences muscle blood flow. Overall, it puts the body under stress and enhances alertness and readiness for action, aka fight or flight.
- Parasympathetic Nervous System: The parasympathetic nervous system is the “counterpart” of the sympathetic system. It slows down bodily functions, leading to a state of “rest and digest.” It lowers heart rate and blood pressure and initiates a phase of recovery and relaxation.
- Enteric Nervous System: The enteric nervous system controls the functions of the digestive tract, including digestion, nutrient absorption, and elimination.
Important neurotransmitters and hormones of the autonomic nervous system [6]:
- Adrenaline (Epinephrine): Adrenaline is a stress hormone and neurotransmitter, and, for example, increases heart rate.
- Noradrenaline (Norepinephrine): Noradrenaline is a hormone and neurotransmitter as well and stimulates blood vessels to constrict, for example.
- Acetylcholine: Acetylcholine is a neurotransmitter that influences sweat production and sleep patterns, sensitizes pain receptors, and mediates signals between nerves and muscles.
Types of Dysautonomia [7]
The most common forms of autonomic neuropathy/dysautonomia that can occur alongside the Ehlers-Danlos syndromes are orthostatic hypotension (OH), postural orthostatic tachycardia syndrome (PoTS), and neurocardiogenic syncope [8].
PoTS (Postural Orthostatic Tachycardia Syndrome): PoTS is characterized by a rapid increase in heart rate when an affected individual gets into an upright position. An increase of over 30 bpm (beats per minute) when transitioning from a lying to a standing position or an increase of over 120 bpm is considered pathological.
Neurocardiogenic Syncope (also known as Neurally Mediated Syncope, Neurally Mediated Hypotension): Neurocardiogenic syncope is the most common form of dysautonomia and refers to a temporary loss of consciousness due to the accumulation of blood in the legs when in an upright position.
Multiple System Atrophy: Multiple system atrophy is similar to Parkinson’s disease and is classified as a neurodegenerative disorder. It is also a primary dysautonomia.
Sinus Tachycardia: Sinus tachycardia is defined by a resting heart rate of over 100 beats per minute without physical exertion.
Pure Autonomic Failure (PAF): Pure Autonomic Failure is classified as a primary dysautonomia and is a degenerative disorder of the peripheral nerves.
Autoimmune Autonomic Ganglionopathy (AAG): Autoimmune autonomic ganglionopathy is, as the name suggests, an autoimmune disorder that targets the body’s autonomic ganglia.
Autonomic Dysreflexia (AD): Autonomic dysreflexia is associated with spinal cord injuries.
Baroreflex Failure: The baroreflex is part of the mechanisms that help maintain a stable blood pressure. If the baroreflex fails, dysautonomia develops.
Diabetic Autonomic Neuropathy: Diabetic autonomic neuropathy is one of the most common forms of dysautonomia. It occurs primarily in individuals with diabetes and can lead to neuropathy of the autonomic nerves.
Familial Dysautonomia: This form of dysautonomia is extremely rare and an inherited condition.
Reflex Sympathetic Dystrophy (Complex Regional Pain Syndrome, CRPS): CRPS is primarily considered a pain disorder, but some experts also believe it is a form of dysautonomia.
Orthostatic Hypotension (OH): In orthostatic hypotension, the blood pressure drops when an affected individual gets in an upright posture. OH is defined by a systolic blood pressure drop of 20 mmHg or a diastolic drop of 10 mmHg. Orthostatic hypotension frequently occurs with PoTS in individuals with EDS.
At this point, it is known that people with Ehlers-Danlos syndrome, particularly hEDS, show a greater prevalence of dysautonomia, oftentimes in combination with mast cell activation. However, the mechanism behind it has yet to be fully studied or proven. Varying scientists suggest different ways of how EDS may lead to different types of dysautonomia. A study by De Wandele et al. [9] speculates that the cause of dysautonomia in EDS could be a combination of cardiovascular and sudomotor dysfunction. Other factors such as neuropathy, tissue elasticity, and various medications could additionally influence the development of dysautonomia. As early as 2002, Gazit et al. [10] published a study that established a connection between joint hypermobility syndrome (now HSD) and PoTS. This group suggested peripheral neuropathy or blood pooling in the legs as causative factors. Overall, their autonomic tests indicated sympathetic dysregulation. The review paper on dysautonomia from the NY classification meeting also mentions Chiari and CCI as potential causes [11]. Additionally, various scientists discovered autoantibodies against different receptors, suggesting that a small portion of individuals with PoTS may have an underlying autoimmune condition [12].
Symptoms, Triggers & Causes
Depending on the type of dysautonomia, symptoms can affect the entire body. Some of the common symptoms [13] include:
- Fatigue and exhaustion
- Dizziness and lightheadedness
- Headaches
- High heart rate
- Low blood pressure
- Shortness of breath
- Bladder issues (overactive bladder, urinary retention, urgent urination)
- Gastroparesis, irritable bowel syndrome
- Excessive sweating or no sweating at all
- Heat and cold intolerance
- Cold extremities
- Nausea, vomiting
- Blurred vision
- Difficulty concentrating
|
Digestion |
Heart rate/blood pressure |
Bladder |
Temperature regulation |
|---|---|---|---|
|
Gastroparesis/irritable bowel syndrome |
Rapid heartbeat, low blood pressure |
Urinary retention |
Excessive sweating/no sweating |
|
Diarrhea/Constipation |
Dizziness, headaches, fainting |
Urgent urination |
Cold limbs |
|
Abdominal pain, nausea |
Brain fog, difficulty concentrating |
Overactive bladder |
Intolerance to cold and heat |
Triggers:
- Dehydration
- Physical exertion
- Infections
- Alcohol and sometimes caffeine
- Emotional stress
- Prolonged standing or quick uprighting from a lying/sitting position
- Warm environments (such as a hot shower or summer temperatures)
- Large meals, as more blood pools in the intestines
Causes:
- Diabetes
- Multiple sclerosis
- Parkinson’s disease
- Autoimmune disorders
- Alcohol abuse
- Various medications
- Spinal cord injuries
- Infections
- (Connective tissue disorders)
- (Mast cell activation syndrome)
- Connective tissue disorders and MCAS are comorbid conditions, and as mentioned above, it is not clear whether they cause, contribute to, or how they are associated with dysautonomia.
Diagnostics [14]
Routine Screening:
Tests that can be done by a PCP or regular lab and don’t necessarily require a specialized center are:
- Holter monitoring and echocardiogram to rule out heart disease
- Schellong test: After applying a blood pressure cuff and a pulse oximeter, the patient rests for 15 minutes in a supine position. During the last five minutes of the resting phase, blood pressure and heart rate are recorded every minute. Then, patients get into an upright, free-standing position and remain in that position for ten minutes. During this time, heart rate and blood pressure are measured and documented every minute. This test can easily be done by a primary care physician, and if it is pathological, patients can already start treatment before they see a specialized dysautonomia doctor. Schellong tests can also be performed by the patients themselves at home. (Take proper precautions for this test: for instance, do not do this alone at home; always have something to hold on to; stop if you feel unwell; have other differential diagnoses, such as heart conditions, excluded.)
- Basic laboratory tests: liver, kidney, and thyroid function tests, HbA1c to rule out diabetes, vitamin B12 and folic acid levels, if necessary, ANA, ANCA, rheumatoid factor for suspected rheumatologic diseases, sodium in 24-hour urine.
- Schirmer test: For the Schirmer test, a small absorbent paper is placed under the lower eyelid to measure tear production. This test is performed when dry eye syndrome or Sjögren’s syndrome (an autoimmune condition that can lead to dysautonomia) is suspected.
Specialized Diagnostics:
- Tilt table test: For the tilt table test, patients are lying down on a mechanical examination table. After, they will be strapped onto that table. Similar to the Schellong test, the resting heart rate and blood pressure are usually continuously monitored during the tilt table test. After the resting period, the table is automatically moved to an upright position where the patient remains for at least ten minutes while their blood pressure and heart rate are recorded at regular intervals.
- Valsalva maneuver: The Valsalva maneuver means patients blow against a resistance of 30 mmHg for approximately 15 seconds while blood pressure and heart rate are monitored throughout.
- Heart rate variability: While patients are lying in a relaxed position, deep inhalation and exhalation are performed while blood pressure and heart rate are measured.
- Muscle contraction of the hands: Patients squeeze an elastic ball or a similar object for an extended period while vital signs are monitored.
- Cold pressor test: For this test, patients immerse their hands in cold water, leading to a rapid increase in blood pressure.
- Quantitative sudomotor axon reflex test (QSART): The QSART is a form of sweat test in which controlled amounts of acetylcholine are applied to the skin via a small capsule. The stimulated sweat production is then measured.
- Thermoregulatory sweat test: The patients lie down in a room heated to 40 or 50 degrees Celsius. An indicator powder on the skin shows whether sweat is being produced.
- Sympathetic skin response: Electrodes are placed on both sides of the hand or on the inside of the forearm, at the lower end of the leg, or on the upper part of the foot. External stimuli, such as small electric shocks, are used to stimulate sweat production.
- Skin biopsy: A small amount of skin might be investigated in case small fiber neuropathy is suspected.
- Gastric emptying study if a comorbid gastroparesis is suspected.
- Specialized laboratory diagnostics: Noradrenaline and adrenaline can be measured in blood plasma taken in a supine position and compared with the same parameters taken in an upright position; additionally, ganglionic acetylcholine receptor antibodies and other antibodies can be tested for; and if a rheumatologic cause is suspected, special blood markers can be measured too.
A combination of several of these tests is used to classify which form of dysautonomia a patient might have.
Management [15]
In the case of secondary dysautonomias, the underlying cause must be treated if possible, for instance, diabetes. For secondary dysautonomias or when the underlying cause cannot be treated, different management approaches, consisting of a combination of conservative measures and medication, are utilized.
Conservative Measures:
- Avoidance of triggers: For instance, this could mean avoiding hot environments or hot showers, specific food, some medication, stress, prolonged standing, large meals, and more.
- Increased salt intake: Lots of products can be used to increase salt intake, for example, Nuun tablets. More tips, especially for the hot summer months, can be found here: https://www.chronicpainpartners.com/pots-eds-and-the-scorching-sun-heat-intolerance-your-summer-survival-guide/
- Elevating the head while sleeping: This can help with blood circulation and reduce symptoms when waking up. After waking up, getting up very slowly and cautiously helps, too. (Also, in case of underlying CCI, be careful with head posture.)
- Calf muscle and endurance training: Helping the muscles pump back blood from the legs to the brain by training the calf muscles or starting with careful cardio exercises, for instance, with a recumbent bike, may reduce symptoms long-term.
- Compression stockings or socks and other compression bandages: Compression can help with blood circulation, particularly in the legs, but stomach binders can be used, too, which may be helpful, especially after meals.
- Calming the autonomic nervous system: Many techniques can be used to calm the autonomic nervous system, for instance, meditation, deep breathing, muscle relaxation, and biofeedback. More tips can be found here: https://www.chronicpainpartners.com/ai-meets-medicine-can-chatgpt-unlock-answers-to-your-medical-questions/
Medication:
If conservative measures aren‘t enough, some medication may help reduce symptoms, too. However, most are used off-label, which means they are not authorized for the treatment of dysautonomia. In addition, carefully evaluate possible side effects that might interfere with other comorbid conditions. All new medical treatments, particularly if they involve medication, should only be started under medical supervision and after carefully discussing with your doctor.
- Vasoconstrictors like midodrine
- Fluid-retaining medications like fludrocortisone
- Beta-blockers and other meds that stabilize heart rate, such as propranolol
- Other medications such as Clonidine, Ivabradine, Mestinon
- For patients with autoimmune causes, immunomodulatory treatment such as intravenous immunoglobulin (IVIG) may be considered.
Other newer treatments (which are currently in trials) are transdermal vagus nerve stimulators.
Dysautonomia & Emergencies [16]
Some medications are not well tolerated by people with dysautonomia (but might become necessary to treat other comorbid conditions of EDS, for example, MCAS). In these circumstances, benefits and disadvantages need to be carefully weighed against one another with your treating medical professional. In general, it is important to ensure adequate fluid intake. Electrolyte-rich drinks can help after acute loss of consciousness.
Medications that may not be well-tolerated by people with dysautonomia include (this list is not exclusive, and please note that with the EDS/dysautonomia patient population, there are always many individual aspects to consider):
- Vasodilators
- Narcotics such as codeine, morphine, oxycodone, phenothiazines
- Antiemetics like Phenergan or Compazine
- Niacin
- Nortriptyline
- Amitriptyline or tricyclic antidepressants
- Epinephrine and adrenaline (however, those may be needed for acute anaphylactic reactions in MCAS)
In the case of surgery, the following should be considered:
- Due to the dysfunction of the autonomic nervous system, the body temperature cannot be regulated well in dysautonomia patients, which can quickly lead to hypo- and hyperthermia during and after surgery. Constant temperature control should be maintained.
- Heart rate and blood pressure should be monitored regularly and more frequently than in healthy individuals, especially during positional changes.
- Epinephrine should be avoided as it can worsen tachycardia (but may become necessary for anaphylaxis in MCAS patients).
- Extra fluids and vasopressors should be readily available.
- There may be prolonged periods of hypotension during surgery.
- Avoid thiopental and ketamine; propofol may be better, but caution is advised due to the risk of hypotension.
Helpful Resources
http://www.dysautonomiainternational.org and https://vimeo.com/dysautonomia
Or check out our webinars: https://www.chronicpainpartners.com
Downloadable E-Book (PDF)
Sources
[1] NIH, n. d. Dysautonomia. Online: https://www.ninds.nih.gov/health-information/disorders/dysautonomia#:~:text=Dysautonomia is a disorder of parasympathetic parts of the ANS. [Accessed June 12, 2023]
[2] The Dysautonomia Project, n. d. Identifying Dysautonomia. Online: https://thedysautonomiaproject.org/identifying-dysautonomia/ [Accessed June 12, 2023]
[3] Sandring, S. (2004). Gray’s Anatomy: The Anatomical Basis of Clinical Practice, English (39. Aufl.). Churchill Livingstone.
[4] Goldstein D. S., & Smith, L. (2002). The NDRF handbook for patients with dysautonomias. http://www.ndrf.org/NDRFHandbook.htm.
[5] Waxenbaum, J. A., Reddy, V., & Varacallo, M. (2019). Anatomy, autonomic nervous system. In StatPearls. StatPearls Publishing, Treasure Island (FL); 2021. PMID: 30969667.
[6]
Waxenbaum, J. A., Reddy, V., & Varacallo, M. (2019). Anatomy, autonomic nervous system. In StatPearls. StatPearls Publishing, Treasure Island (FL); 2021. PMID: 30969667.
Vernino, S., Bourne, K. M., Stiles, L. E., Grubb, B. P., Fedorowski, A., Stewart,
J. M., Arnold, A. C., Pace, L. A., Axelsson, J., Boris, J. R., & Moak, J. P. (2021). Postural orthostatic tachycardia syndrome (POTS): State of the science and clinical care from a 2019 National Institute of Health Expert Consensus Meeting. Autonomic Neuroscience, 102828.
Low, P. A. (Hrsg.). (2011). Primer on the autonomic nervous system. Academic.
[7]
Dysautonomia International. http://www.dysautonomiainternational.org
Biggers, A., & Newman, T. (2017). What’s to know about dysautonomia? Medical News Today. https://www.medicalnewstoday.com/articles/76785.
[8] Hakim, A., O’Callaghan, C., De Wandele, I., Stiles, L., Pocinki, A., & Rowe, P. (2017). Cardiovascular autonomic dysfunction in Ehlers-Danlos syndrome – hypermobile type. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175(1), 168–174.
[9] De Wandele, I., Rombaut, L., Leybaert, L., Van de Borne, P., De Backer, T., Malfait, F., De Paepe, A. and Calders, P. (2014). Dysautonomia and its under- lying mechanisms in the hypermobility type of Ehlers-Danlos syndrome. Semi- nars in Arthritis and Rheumatism, 44(1), 93–100. WB Saunders.
[10] Gazit, Y., Nahir, A. M., Grahame, R., & Jacob, G. (2003). Dysautonomia in the joint hypermobility syndrome. The American Journal of Medicine, 115(1), 33–40.
[11] Hakim, A., O’Callaghan, C., De Wandele, I., Stiles, L., Pocinki, A., & Rowe, P. (2017). Cardiovascular autonomic dysfunction in Ehlers-Danlos syndrome – hypermobile type. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175(1), 168–174.
[12] Hakim, A., O’Callaghan, C., De Wandele, I., Stiles, L., Pocinki, A., & Rowe, P. (2017). Cardiovascular autonomic dysfunction in Ehlers-Danlos syndrome – hypermobile type. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175(1), 168–174.
[13]
Hakim, A., O’Callaghan, C., De Wandele, I., Stiles, L., Pocinki, A. and Rowe, P., 2017, March. Cardiovascular autonomic dysfunction in Ehlers–Danlos syndrome—hypermobile type. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 168-174).
Raj, S.R., 2013. Postural tachycardia syndrome (POTS). Circulation, 127(23), pp.2336-2342
Dysautonomia International. (2019). Postural Orthostatic Tachycardia Syndrome. Online: http://www.dysautonomiainternational.org/page.php?ID=30. [Accessed 17.08.2021].
[14]
Goldstein D. S., & Smith, L. (2002). The NDRF handbook for patients with dysautonomias. Online: http://www.ndrf.org/NDRFHandbook.htm. [Accessed: August, 2021]
Haensch, C. A., Wagner, C., Mallien, J., & Isenmann, S. (2013). Posturales Tachykardiesyndrom. Nervenheilkunde, 32(04), 199–204.
Jones, P. K., & Gibbons, C. H. (2015). Autonomic function testing: An im- portant diagnostic test for patients with syncope. Practical Neurology,
15(5), 346–351.
Artide, S. (1996). Clinical autonomic testing report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology, 46, 873–880.
Illigens, B. M., & Gibbons, C. H. (2009). Sweat testing to evaluate autonomic function. Clinical Autonomic Research, 19(2), 79–87.
[15]
Goldstein D. S., & Smith, L. (2002). The NDRF handbook for patients with dysautonomias. Online: http://www.ndrf.org/NDRFHandbook.htm. [Accessed August 2023]
Hakim, A., O’Callaghan, C., De Wandele, I., Stiles, L., Pocinki, A., & Rowe, P. (2017). Cardiovascular autonomic dysfunction in Ehlers-Danlos syndrome – hypermobile type. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175(1), 168–174.
Rowe, C. P. (2014). General information brochure on orthostatic intolerance and its treatment. Chronic Fatigue Clinic Johns Hopkins Children’s Center.
[16]
Mustafa HI, Fessel JP, Barwise J, Shannon JR, Raj SR, Diedrich A, Biaggioni I, Robertson D. Dysautonomia Perioperative Implications. The Journal of the American Society of Anesthesiologists. 2012 Jan 1;116(1):205-15.
Corbett WL, Reiter CM, Schultz JR, Kanter RJ, Habib AS. Anaesthetic management of a parturient with the postural orthostatic tachycardia syndrome: a case report. British journal of anaesthesia. 2006 Aug 1;97(2):196-9.
Rabbitts JA, Groenewald CB, Jacob AK, Low PA, Curry TB. Postural orthostatic tachycardia syndrome and general anesthesia: a series of 13 cases. Journal of clinical anesthesia. 2011 Aug 31;23(5):384-92.