
Special thanks to EDS medical provider Pradeep Chopra, MD for reviewing this article curated by our media team. Learn more from his expertise in his video webinar on EDS Pain Management (discussion on tethered cord at the 1:13 mark).
Intro: Hope for Tethered Cord Syndrome Patients
Tethered Cord Syndrome (TCS) is a common condition found in patients with Ehlers-Danlos syndrome (EDS) that, as of today, is very little known or understood. So, our Chronic Pain Partners media team set out to outline the condition as it relates to EDS in this article. We learned from research and provider interviews that there is good news on the horizon for patients who are curious or seeking diagnosis and treatment. This is not medical advice and should not be used in place of a doctor.
The best news in the medical community is when a condition reaches a level of commonality in the patient population to be studied by medical researchers and published in a peer-reviewed journal, where TCS currently is. Also, great news is that treatment options are very effective and can give people reduced pain and better mobility, especially with improved walking. It’s not often a doctor can tell an EDS patient that the outcome is consistently effective, so let’s pause for a moment to celebrate that! Yes, there is hope coming for those who might be frustrated with the lack of tethered cord information, resources, and expert provider waitlists that are hopefully getting shorter. According to Dr. Chopra during our January 2024 interview, new research studies will be coming out from several EDS-aware surgeons and experts soon. But for now, here are the basics to know about Tethered Cord syndrome.
Know the Basics: Normal Anatomy of Lower Lumbar Spine
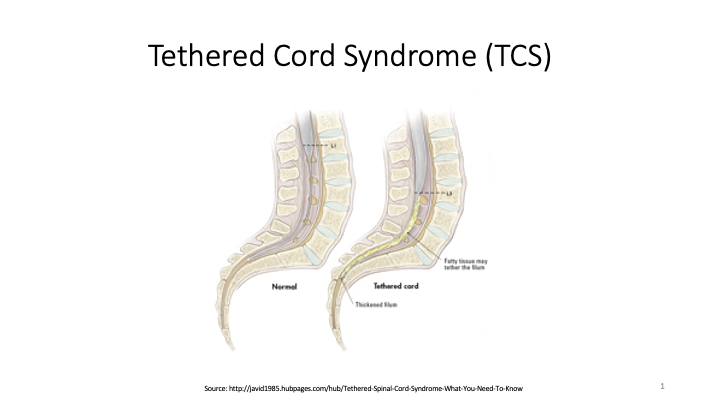
Although the entire spinal cord can be impacted, the focus is primarily on the lumbar or pelvis region of the spine. According to Dr. Chopra, the spinal cord comes out of the brain stem and ends at the other end of the spine around the L1 level. Here, there’s a piece of tissue hanging loose called the Filum Terminale that aids in stabilizing the spinal cord. This is the part that gets released during potential release surgery, so rest assured without fear that a release procedure does not involve any form of cutting the spinal cord, which is often a valid patient’s fear.
Anatomical changes in lower lumbar spine in TCS
What happens in TCS is that the bottom of the filum gets stuck to the lumbar or sacrum area of the spine and the result is the spinal cord itself gets pulled down, thus called “tethered.” A true tethered cord is one that lies below L2, as is the case in spina bifida. This is one of the ways TCS is diagnosed by an MRI – to see where the end of the spinal cord (called a conus) and where it ends (see above image linked to source for variations ending at L1 and L3). Neurosurgeons are looking at the MRI images (not relying on the radiological reports alone) to determine whether the conus is pulled down and where it ends.
In some people with EDS or connective tissue disorders, there is sometimes no evidence of the conus being pulled down, and MRIs show a normal lying-positioned conus at T12/L1. When this happens, it’s called Occult Tethered Cord (OTC), meaning it is hidden. Dr. Petra Klinge, a renowned neurosurgeon treating these highly complex cases, published research on TCS and hypermobile EDS suggesting issues with the filum terminale in hypermobiity prove to be a challenge to correctly diagnose. In these cases, patients are often sent for additional testing for urodynamic studies to evaluate for a potential neurogenic bladder. Another diagnostic method to look for is whether the patient has a fatty or thickened filum. A thickened or fatty filum is known to cause a tethered cord, according to research, but is an expert diagnostic decision. This is the challenge of complicated connective tissue disorders in EDS patients and why it is so hard to diagnose, with so few experts understanding the nuance of hypermobile bodies.
Top 3 Symptoms of Tethered Cord syndrome in EDS
- Complaint of severe back pain, especially low back pain that is not explained by other reasons; plus, weakness and heaviness in legs, that worsen when walking, going up an incline, or stair climbing. Some people also experience pain at the bottom of their feet.
- Irregular pain sensations and muscle spasms in the legs, often occur at different places and vary between the right and left legs.
- Bladder symptoms that lead to neurogenic bladder symptoms where the brain and bladder aren’t communicating such as:
- Incontinence – trouble holding it and urine releasing involuntarily
- Urgency – feeling like you should go immediately
- Frequency – going often, having difficulty feeling like you can’t empty your bladder
- Retention – difficulty relieving yourself without pushing or leaning forward while seated, or urinating infrequently (such as only twice a day)
Other Signs Doctors Look For with TCS
A physical exam will include checking for any low back issues, and looking for neurological symptoms that can also impact function. Then neurosurgeons will order an MRI of the lumbar spine (and possibly the thoracic and cervical spine to rule out any other spine abnormalities) for imaging to review the tail end of the spine for filum abnormalities. Unfortunately, as previously stated, there are few signs to look for and limited medical research, while people present differently with tethered cords at different ages. For example, children may walk on their toes or heal, or in the average patient population, you may see skin changes, hair at the low back, or a deep gluteal crease or dimple that is not always there in everyone.
Potential Correlation Between Inflammation, Mast Cells and TCS
The most important point to be aware of is that not all people with TCS have pain and/or symptoms. Dr. Chopra shared that the reason why TCS symptoms can develop is currently being studied (hopefully with research out soon from EDS expert neurosurgeons) to determine the role mast cells play in developing increasing amounts of inflammation in the filum. Experts are finding cells seen on a microscope of mast cells collecting into the filum. According to Chopra, recently a board of 400 medical experts met to discuss this theory that could offer an explanation for why it’s possible to either have pain or not related to inflammation levels. This dichotomy of having pain and symptoms or not results in only the people who are very symptomatic getting diagnosed, having the surgical procedure, and getting better, but research is pending. Plus, the challenge of Occult Tethered Cord as outlined in this research. Clearly, no patient or doctor team would do surgery for nonexistent symptoms, so it will likely remain unknown for now.
Diagnostic Tests and Radiological Findings in TCS
See a neurosurgeon, preferably an EDS knowledgable one, who will typically order the following testing:
- Multiple MRIs (without contrast) for cervical, thoracic, and lumbar spine to see the whole spine to rule out anything else causing symptoms. The lumbar MRI is the most critical imaging to evaluate and diagnose TCS. Some neurosurgeons will also order a prone lumbar MRI (on your belly, face down) to see if the filum defies gravity, because it can be seen staying up against the back and not falling forward with the rest of the spinal cord. That view can sometimes show a tethered cord correctly and also show retethering from a previous TCR.
- A urodynamic study conducted by a urologist who will be looking for neurogenic bladder symptoms and if the sphincter is strong enough to handle potential incontinence. It’s important to note, the urologists do not diagnose or comment in their report/evaluation on the presence of TCS or not, only remarking if neurogenic bladder exists (meaning there’s brain communication irregularities with the bladder). The urodynamic study has patients seated with a catheter for various voluntary urinary activities while an ultrasound measures as the bladder fills. Always let your neurosurgeon interpret the urodynamic study results.
Treatment and Outcomes
Before considering surgery, many alternative methods can help address pain, including physical therapy and injections, especially with a specialist in hypermobility and pelvic floor issues. But if it seems surgical intervention is your best option for safe spine stability and/or pain relief and mobility, let’s outline the basics of the procedure to repair a tethered cord in a hypermobile body.
First, calm any fears you might have about the potential surgery called Tethered Cord Release (TCR) because there is no actual spinal cord being cut, which is a common patient concern that leads many people to avoid treatment. During the procedure, neurosurgeons remove the back of the vertebra bone (called a laminectomy) to gain access to your spinal canal by opening the dura. Since the dura is opened during the procedure, it is usually required for patients to lie flat for 1-3 days in the hospital post-op to recover and not cause any cerebral spinal fluid (CSF) leaks while healing, and then it’s usually safe to move.
Surgery outcomes for most patients see an immediate restoration of a normal functioning bladder within a few days, while leg pain can take longer, and improvements continue for up to a year after the procedure. Success rates are researched, and results are 48–100% effective. The spinal cord does have the potential to re-tether after surgery, as noted in research and in many patients who are hypermobile, though. For this reason, follow-up care is critical after tethered cord surgery, but overall, TCR procedures show good, lasting results for most patients.
Other Considerations and Comorbidities
One study by one of the EDS expert neurosurgeons, Dr. Paolo Bolognese concluded that 66% of patients with Chiari Malformation also have TCS. Chiari formation has been frequently identified in association with the tethered cord according to at least two studies (link 1 and link 2). The general understanding has been that the tethering of the cord is the primary issue that results in “pulling” of the spinal cord at the brain stem causing Chiari. The concluding recommendation is anyone with Chiari Malformation get evaluated for TCS and vice versa.
The determination of if you have tethered cord or not is definitely a clinical diagnosis made only by a trained medical professional with expertise in this area. While this article might provide some symptomatic overviews and guidance on the types of tests that may be ordered by your neurosurgeon, trust this level of care only to the doctors who know best (our media team is not medically trained).
Hold onto hope if you are seeking treatment because surgical intervention for TCS can offer pain relief, improved quality of life, and improvements in walking for many EDS patients.
Bibliography:
Henderson, Fraser C., et al. “Neurological and Spinal Manifestations of the Ehlers–Danlos Syndromes.” American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 21 Feb. 2017, <www.onlinelibrary.wiley.com/doi/10.1002/ajmg.c.31549/full>.
“Section of the Filum Terminale Surgery for Tethered Spinal Cord Syndrome in Patients with Chiari Malformation and Syringomyelia.” North Shore-Long Island Jewish Health System The Chiari Institute, Chiari Connection International, 02 Oct. 2006, <http://www.chiariconnectioninternational.com/docs/TCS_SFT_Explained.pdf>.
Quake. “Overview: Chiari Comorbidities & Etiological/Pathological Cofactors [Revised].” Chiari Bridges, 16 Nov. 2019, https://chiaribridges.org/overview-chiari-comorbidities-etiological-pathological-cofactors/.
Arslanoglu, A., et al. “Multidisciplinary Combined Approach for Tethered Spinal Cord Syndrome: Radiology, Surgery and Physical Therapy.” Balkan Military Medical Review, 2006, https://pdfs.semanticscholar.org/8c30/18bf5bfbd6f3e7e5e9c3559bbbfdcac82e04.pdf.
Milhorat, Thomas H., et al. “Association of Chiari malformation type I and tethered cord syndrome: preliminary results of sectioning filum terminale.” Surgical Neurology, Elsevier, July 2009. https://www.sciencedirect.com/science/article/abs/pii/S0090301909002572.
Aoun, Salah G., et al. “The Use of Prone Magnetic Resonance Imaging to Rule Out Tethered Cord in Patients With Structural Spine Anomalies: A Diagnostic Technical Note for Surgical Decision-making.” Cureus vol. 11,3 e4221. 11 Mar. 2019, doi:10.7759/cureus.4221. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6510567/.



I am just letting you know that tight filum terminal/tethered cord syndrome in EDS patients has many other neurological complaints, as detailed in the recent paper by; Klinge, P. M., Srivastava, V., McElroy, A., Leary, O. P., Ahmed, Z., Donahue, J. E., Brinker, T., De Vloo, P., & Gokaslan, Z. L. (2022). Diseased Filum Terminale as a Cause of Tethered Cord Syndrome in Ehlers-Danlos Syndrome: Histopathology, Biomechanics, Clinical Presentation, and Outcome of Filum Excision. World neurosurgery, 162, e492–e502. https://doi.org/10.1016/j.wneu.2022.03.038
Thank you for sharing this research. We will add it to the article.