Understanding Tethered Cord Syndrome and Occult Tethered Cord in Ehlers-Danlos Syndrome

Unravelling Tethered Cord with EDS: A Patient Guide
(Also see the simplified version of this article)
Unravelling the tethered cord has proven to be an elusive topic. Basically, there is not a great deal of credible insight or medical research available on it. To start simply, we begin with basic anatomy and symptoms most commonly seen by doctors to help you better understand the complex medical condition with a challenging diagnostic journey.
In short, Tethered Cord Syndrome (TCS) revolves around the undue stretching of the spinal cord, resulting in numerous neurological complications and pain. TCS can impact functioning as this part of the body serves as a relay station between the brain and the rest of the body and is responsible for several autonomic functions involved in such fundamental processes as breathing, sleeping, and sensory and motor functions, so it is critical to get evaluated by an expert.
- *Respiratory function
- *Sleep and arousal
- *Sensory and vestibular balance
- *Motor functions (including regulation of processes like chewing, salivation)
- *Origin of Cranial Nerves: Trigeminal nerve, Abducens nerve, Facial nerve Vestibulocochlear nerve
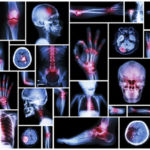
Back to Basics: The Anatomy of The Human Spine
- *The vertebral column plays a pivotal role in sustaining an upright spine while shielding the spinal cord from injuries. It comprises thirty-three vertebrae.
- *The upper twenty-four vertebrae have intravertebral discs, rich in collagen- a known trouble spot of faulty protein in hEDS. These discs normally functioning grant flexibility to the vertebral column.
- *The spinal canal envelops the spinal cord in cerebrospinal fluid, safeguarding it from damage and providing essential nutrients. The outermost layer of the meninges, making up the spinal canal, is the dura mater.
- *The spinal cord acts as the communication bridge between the brain and the body’s nerves.
Tethered Cord Syndrome and its Association with EDS
Tethered Cord Syndrome occurs when the filum terminale adheres to either scar tissue or the dura lining of the spinal canal. “Dura,” is one of the three layers of membranes (meninges) that surround and protect the brain and spinal cord. While it can emerge at any spinal canal point, its prevalence is higher at the lumbosacral level (low back). Patients with conditions like Spina Bifida, Spina Bifida Occulta, and some patients with hypermobility and/or Ehlers-Danlos Syndromes (EDS) are more prone to tethered cord. Tethered Cord happens when the sticky fibrous tissue of the filum adheres to fatty/scar tissue or the dura lining of the spinal canal. While this tethering can happen anywhere in the spinal canal, it is most common at the lumbosacral level often felt in the low back/sacrum/tailbone area. When the tethered filum pulls the spinal cord tightly enough that it causes neurological problems, it becomes known as Tethered Cord Syndrome (TCS).
Identifying Symptoms of Tethered Cord Syndrome
Detecting TCS can be extremely challenging due to its elusive nature. You may get different diagnosis from different medical experts based on their clinical diagnosis. While some individuals may exhibit clear signs of TCS, others may not. Hence, being familiar with all potential symptoms is crucial. But often the signs can go unnoticed, as is the case with difficult-to-diagnose occult tethered cord.
Occult Tethered Cord Syndrome (OTCS) is a condition in which the spinal cord becomes attached to the spine, preventing it from moving freely within the spinal canal. “Occult” in this context means “hidden,” suggesting that the tethering may not be immediately obvious on standard imaging studies like MRIs and even harder to diagnose and prove to health insurance providers the necessity of treatment or surgical intervention. Patients with hypermobile Ehlers-Danlos Syndrome (hEDS), can sometimes present with neurologic symptoms that might be consistent with OTCS, although the connection between hypermobility and tethered cord remains a topic of study and debate.
In hypermobile individuals, or those with EDS, who suspect they may have OTCS, the following symptoms might be observed:
Symptoms:
- *Pain: Chronic back pain, especially in the lower back. This pain may worsen with activity or straining, walking or stair climbing.
- *Muscle Weakness or numbness in the lower limbs
- *Urinary issues such as:
- Incontinence-trouble holding it
- Urgency- feeling like you should go immediately
- Frequency-going often
- Retention-difficulty relieving yourself without pushing or leaning forward while seated
- *Muscle spasms: This can include leg or foot cramps.
- *Gait Abnormalities: Changes in the way a person walks, such as foot drop or a shuffling gait.
- *Deterioration of Motor Skills: This can manifest as clumsiness or coordination issues.
- *Orthopedic Abnormalities: Such as scoliosis or foot deformities.
However, as always, diagnosing OTCS—especially in the context of another complex condition like hEDS—can be challenging. It requires a comprehensive clinical evaluation and collaboration between various specialists, which are very rare and challenging to get appointments with due to long wait times.
Medical Specialists to Consult
- *Neurologist: Can provide an initial evaluation of symptoms and guide towards further diagnostic tests.
- *Neurosurgeon with TCS experience: Not all neurosurgeons are familiar with the subtleties of TCS, especially occult tethered cord. It’s essential to seek a neurosurgeon who has experience with this specific condition. There are very few hypermobile-aware neurosurgeons in the US that can evaluate, diagnose, and treat TCS.
Diagnostics Imaging and Testing
- *Magnetic Resonance Imaging (MRI): The first diagnostic step is typically a lumbar MRI. While tethering might not always be directly visible, its impact on the spinal cord can be seen. MRIs can be done supine (lying down) or prone (face down), or both can help detect tethering due to the spinal cord’s positioning when lying down on your back, where it can appear normal.
Sometimes radiological criteria are not met or are ambiguous, yet an Occult Tethered Cord (characterized by the presence of symptoms with normal conus position and inconclusive findings of the filum) can still exist. Other signs of tethering that might be visible in a lumbar MRI include an enlarged foramen magnum, thick or fatty filum, presence of fatty tissue inside the canal, or the filum might be pulling to one side of the spinal canal. A prone MRI of the lumbar region can be an invaluable tool for those where other MRIs indicate that the filum might be pulling to one side (usually the back side) of the canal. With prone MRIs, imaging is done while the patient is lying face down (as opposed to facing up, like most supine MRIs). Some neurosurgeons prefer to see prone images to better visualize any tethering as the filum defies gravity.
- Other Diagnostic Tests:
- *Electromyogram (EMG) Test and Nerve Conduction Study (NCS): Recommended for thorough evaluation of the nerve function in the lower limbs.
- *Urodynamic Study: Important for analyzing the function of the bladder and its associated structures for any neurological changes. These invasive tests can determine if the patient has symptoms of a neurogenic bladder measuring the amount of liquid your bladder can hold measured at intervals on when your nerve signals release.
- *Cervical MRI: This can show the spinal cord to be abnormally tight and potentially show signs that a tethered cord might exist. The cervical spinal cord can sometimes be seen as narrow from it being pulled tight.
Patience is Key to Diagnosis
Even with the correct imaging and every symptom listed, patients are often told they do not have Tethered Cord. Therefore, it is important to make sure that you have the images viewed by a neurosurgeon that is familiar not only with TCS and EDS. The combination of the images and the patient’s symptoms should tell the neurosurgeon if surgical intervention is required
Tethered Cord Treatment Options
- Conservative Approach: Physical therapy, pain management, and medications can help alleviate some symptoms. Some patients can get relief from temporary measures such as steroid or regenerative therapy injections (prolotherapy or PRP) in the short term. However, when your medical team have determined true tethering, surgical intervention usually becomes necessity.
- Tethered Cord Release (TCR) Surgery: Some patients are ultimately needed to be surgically treated with a Tethered Cord Release, involving the untethering of the spinal cord. An incision is made in the lumbar area of the low back.
Surgical treatment is not without risk and does not guarantee relief of symptoms. There is usually a prescribed minimum of 24 hours flat on your back immediately post-op during your hospital stay to reduce potential cerebral spinal fluid (CSF) leaks. Most patients describe the surgery as a painful recovery for only the first two weeks and “better than they ever remember feeling” (often because they have been tethered for much of their lives). In a large study by the NIH, up to 83% of adult patients report relief, 16% unchanged, and 1% report feeling worse. In children, the numbers are even better with 93% obtaining improved symptoms and 7% unchanged. Another study concludes a success rate of 48-100%.
- Shunt placement: In cases where a cyst or syrinx develops, a shunt might be placed to drain excess cerebrospinal fluid.
Risks to Consider Before Tethering Release Surgery
Here’s an outline of the risks and complications associated with Tethered Cord Release (TCR) surgery, particularly in EDS patients:
1. Retethering: This occurs when the spinal cord adheres again to its surrounding structures after being surgically released with a higher likelihood of poor wound healing and scar tissue formation.
2. Cerebrospinal Fluid (CSF) Leak: CSF leak happens when there’s an unintentional opening in the dura mater, the protective covering of the brain and spinal cord, leading to leakage of the CSF.
3. Intracranial Hypertension (IH): A condition where the pressure inside the skull (intracranial pressure) is increased. It’s not directly a complication of surgery but can be associated with conditions like CSF leaks, Chiari and hypermobile EDS.
4. General Surgical Risks in EDS:
- Poor wound healing: The skin of EDS patients may not heal as efficiently as others resulting sometimes in wounds reopening or healing with widened or atypical scars.
- Excessive bleeding: Abnormal connective tissue can make vessels more fragile, leading to increased intraoperative and postoperative bleeding.
- Anesthetic complications: There’s some evidence to suggest that EDS patients might be at a higher risk for complications with certain anesthetics.
Conclusion
The determination of whether you have a tethered cord or not is definitely a clinical diagnosis made only by a trained medical professional with expertise in this area. Different neurosurgeons may also have differing interpretations and, thus, different diagnosis. SO you can see why this diagnostic journey can be so challenging for patients. While this article might provide some symptomatic overviews and guidance on the types of tests that may be ordered by your neurosurgeon, trust this level of care to the doctors who know best. Hold onto hope if you are seeking treatment because surgical intervention for TCS can offer pain relief, improved quality of life, and improvements in walking for many EDS patients.
Bibliography & Sources Cited:
Henderson, Fraser C., et al. “Neurological and Spinal Manifestations of the Ehlers–Danlos Syndromes.” American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 21 Feb. 2017, <www.onlinelibrary.wiley.com/doi/10.1002/ajmg.c.31549/full>.
“Section of the Filum Terminale Surgery for Tethered Spinal Cord Syndrome in Patients with Chiari Malformation and Syringomyelia.” North Shore-Long Island Jewish Health System The Chiari Institute, Chiari Connection International, 02 Oct. 2006, <http://www.chiariconnectioninternational.com/docs/TCS_SFT_Explained.pdf>.
Quake. “Overview: Chiari Comorbidities & Etiological/Pathological Cofactors [Revised].” Chiari Bridges, 16 Nov. 2019, https://chiaribridges.org/overview-chiari-comorbidities-etiological-pathological-cofactors/.
Arslanoglu, A., et al. “Multidisciplinary Combined Approach for Tethered Spinal Cord Syndrome: Radiology, Surgery and Physical Therapy.” Balkan Military Medical Review, 2006, https://pdfs.semanticscholar.org/8c30/18bf5bfbd6f3e7e5e9c3559bbbfdcac82e04.pdf.
Milhorat, Thomas H., et al. “Association of Chiari malformation type I and tethered cord syndrome: preliminary results of sectioning filum terminale.” Surgical Neurology, Elsevier, July 2009. https://www.sciencedirect.com/science/article/abs/pii/S0090301909002572.
Aoun, Salah G., et al. “The Use of Prone Magnetic Resonance Imaging to Rule Out Tethered Cord in Patients With Structural Spine Anomalies: A Diagnostic Technical Note for Surgical Decision-making.” Cureus vol. 11,3 e4221. 11 Mar. 2019, doi:10.7759/cureus.4221. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6510567/.