Rising Doctor Making an Impact on hEDS: Q&A with MUSC MD/PhD Student Roman Fenner
In this interview, Christie Cox speaks with a rising doctor who also has hEDS and other comorbidities, Roman Fenner. Fenner is currently enrolled in the Medical University of South Carolina (MUSC) as a dual enrollment student for an MD and PhD – meaning he will learn how to lead medicine and science combined in an intensive NIH-funded program teaching both clinical care of patients and scientific research simultaneously. He was also one of the first four inaugural interns at the MUSC Norris Lab in 2021 when they made their discovery (pending research publication), so he has been on the exciting frontier for years beyond his own patient story. Read the Q&A to learn more about what he is doing now and where he thinks the future of connective tissue disorders, diagnostics, treatment and care could go.
Christie Cox:
Thanks for being with us today. My name is Christie Cox. I’m the author of the book on how to deal and heal with hypermobile EDS called “Holding It All Together When You’re Hypermobile.” I also occasionally have the opportunity to help the Chronic Pain Partners volunteer media team spread EDS awareness. Today we’re doing just that with sharing hope for hypermobility with a preview to the future of medicine and science around hypermobile Ehlers-Danlos syndrome (hEDS) with our invited guest Roman Fenner. He is a medical student, EDS patient and a brilliant advocate who is making such an impact in his own life and the people around him at MUSC. We want to find out what he’s up to what he sees as hope on the horizon for the future for hypermobility. So welcome, Roman. Thanks for being here.
Roman Fenner:
Thank you so much for having me, Christie. It’s an honor.
Christie:
Can you give us a brief introduction about yourself, where you are in your student career and how it relates to medicine and hypermobile EDS?
Roman:
Absolutely. I’m Roman Fenner. I’m 23 years old, and I have hypermobile EDS. I was diagnosed when I was nine years old, which is far earlier than the majority of people diagnosed with it. That was due to me having family members who were far sicker than I was at that point. And because it’s a genetic disease, we all got diagnosed together. Even though I wasn’t too symptomatic at the time, I was very bendy. I didn’t have comorbidities at that point, which came later— including Chiari, cranio-cervical instability, tethered cord, and POTS. Back then, I was very active. I was in athletics, scouts and Taekwondo. Then the geneticist told me “You have to quit all of these things because once you hit puberty, they’re going to destroy your body.” I did drop those things, but my body fell apart years later regardless. So in about a year and a half, I had 10 (mostly) neurosurgeries and procedures to put my body back together.
All these things came on and hit me like a truck when I was 16. I was treated for cranio-cervical instability with a skull-to-C2 spinal fusion, I had tethered cord surgery, and a VP shunt all back-to-back. There’re a lot of different reasons why that could have happened – part because of hormones, but it was then that I decided I wanted to be a doctor. I had begun to take a bunch of AP classes and was reading textbooks every night. I was craning my neck down in horrible positioning and other things that a normal person might do. But in somebody who was super bendy like me, I was destroying my ligaments in the process. It was really debilitating to have all these brain and spine problems like Chiari malformation, intracranial hypertension, getting a VP shunt, that shunt failing a couple of times and getting infected, having more revisions, and even having reconstructive surgery because my scalp didn’t heal properly. It really showed me just how many things can go wrong when you have this disease— that it’s not just a condition that makes you really bendy like a lot of people think.
Some doctors might recall, “When I went to medical school a couple of decades ago, I read one paragraph about people like you— where you can stretch your skin and bend and you’re really good at sports.” It’s far more than that. I saw my family experience that in their trouble getting diagnosed. And then that happened to me. Luckily, I had a great team of specialists because all of these family members had already been treated and had to basically trailblaze before me, so I got the care right when I needed it. That sometimes meant I would be bed-bound, and I did miss a lot of high school. Despite that, I was always either on the way for surgery or was in recovery. And even though something was going wrong, I was always fortunate to have had the right access, so that really inspired me. I came to see this deficit in healthcare.
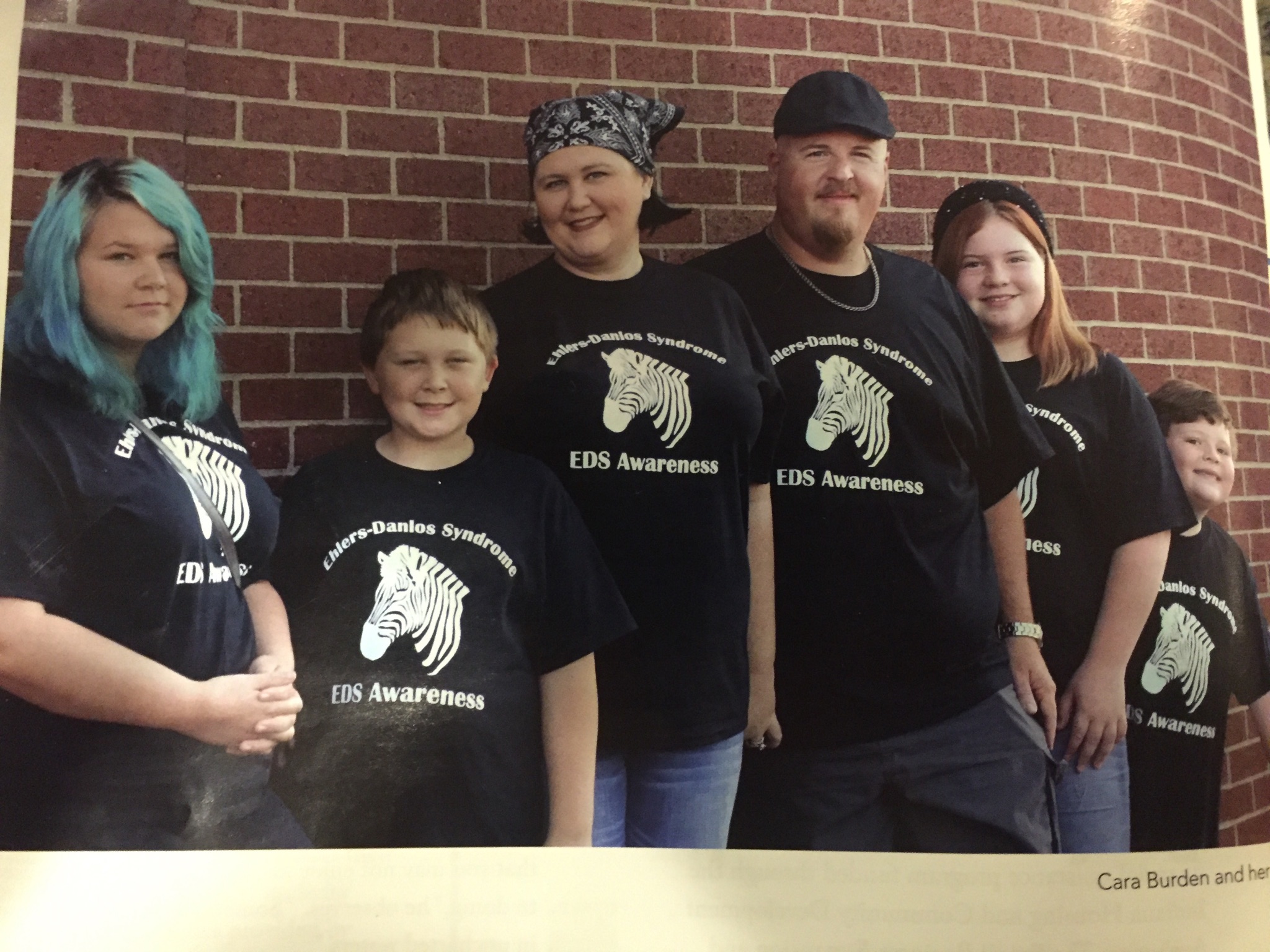
I also saw how there’s such a strong patient community with EDS in general, with all the different subtypes, and with people with chronic disease and disability in general. It taught me a lot about resilience. Plus, there’s this deficit in science and in healthcare, where we don’t really know what causes a lot of these conditions. We just treat them by bandaging you up. We put metal in you and hope you stay together and wait until a couple of months down the line when something else happens— because something will go wrong since your whole body’s falling apart. I’ve loved science since I was a little kid. I always loved problem-solving and wondering why and how things work. I have been involved in the patient community and advocacy, like with the Bobby Jones Chiari and Syringomyelia Foundation along with my mom and sister. One of their first diagnoses was Chiari malformation. It was something that my mom had realized she’d been living with her whole life. My sister had a tethered cord with a lot of complications as a toddler. It became very evident to my parents that she also had Chiari. We all got involved in the community before we knew we even had EDS, and we’re still actively involved in those communities and lead support groups every month. For me, the neurological comorbid conditions are really where a lot of my familiarity and experience rest. Being active in organizations like Bobby Jones CSF has helped me understand the need for medical research for conditions such as Chiari, intracranial hypertension, syringomyelia, CCI, and the list goes on. But I’ve also lived with things like POTS/dysautonomia, and a lot of other associated conditions.
I have been in the patient community as an advocate for almost 10 years now. And being in that community, and already knowing that there’s this issue in science, there’s also an issue with access to care and education. When you have such complex disorders, and you see a new doctor for the first time, you’re just listing off all the surgeries you’ve had, all the conditions you have, you feel like you sound crazy. You feel like you sound like a hypochondriac because you have a long list, but you learn how to live with it. You’re your own advocate. I was fortunate to have physicians and surgeons who were great inspirations and encouragers, supporting my extensive knowledge of my disorders. It’s by patients telling other patients our stories that we’re going to find answers because we know what it’s like to live with this. That idea set me in motion.
In college, I was pre-med and double majored in biology and music. Getting kicked out of sports led me to try music as an extracurricular. I ended up loving that. It gives me a creative outlet during so much hard science and study. So, fast-forwarding, I just started my first year of medical school this past August 2023. I’m in the medical scientist training program at the Medical University of South Carolina (MUSC), which is an NIH-funded MD/PhD dual degree program. It is an honor to be here. It’s a dream come true. I started some preliminary work in the PhD program— kind of just getting acquainted, this past June. Now I’m wrapping up my first block of study in medical school. It’s been a journey, but they did mention EDS in the curriculum which is a good sign for future medical students! They’re teaching us a lot of good tools, such as the idea that “the patients have the answers” and to have humility as doctors. I went in hoping to put those things into practice and am pleased to know that the other 180 people in my class are also being taught these humanistic principles. It is really encouraging for where medicine is going.
Christie:
A little bit of your story is you sought out and got the opportunity to be at the MUSC Norris lab as one of the first hEDS interns in the summer of 2021. Tell me a little bit about that experience, and how it led you to be back at MUSC now.
Roman:
Yeah, it’s instrumental. My personal patient experience was pivotal in helping me realize I needed to pursue medicine. But my experience in the Norris Lab showed me I needed to pursue science as well – probably one of the most important things to happen to me. It helped me realize what I could be doing, and what was possible. For all these years prior, I was just hoping that I could be a compassionate clinician, that even though we don’t have answers, I can just be an encourager and comforter, expressing empathy as a care provider. But being part of the Norris Lab hEDS intern program at MUSC right around the time they found the candidate gene for hEDS was monumental. Together we worked on their EDS mouse model, and they were very clearly exhibiting signs and symptoms of hypermobility in the lab. I remember doing electron microscopy on the collagen fibers of these mice, and they did not look normal compared to regular mice.
Growing up I always wanted to know what caused everything and recall being frustrated not knowing what the cause was with my own conditions going on in my body. Imagine getting to explore those ideas and assumptions in a scientific way? The mentorship with Dr. Norris and Dr. Gensemer showed me what I could be doing in this field— that this internship wasn’t just a one-stop. The purpose of this program, now in its third year, is to generate more physician-scientists, patient-scientists, patient-physicians, advocates and more. It’s an awesome opportunity in research for the patient, community, and education. You see where the future is heading, which hopefully involves an EDS institute being developed at MUSC.
MUSC is leading this long-term groundbreaking hEDS work, but this needs to happen at every other major medical center in the country. If hypermobile EDS/HSD and all its comorbid conditions are more common than diabetes or heart disease, then students at Hopkins, Stanford, Harvard—all these other institutions, need to be aware of the implications of this disease and have a hand in its study. It’s our job to go out and be trailblazers, and the Norris Lab really equips us with that. They’ve helped me realize it’s possible to get a PhD while having these conditions with the right accommodations, and medical school combined with graduate school isn’t as scary or untouchable. It’s a long journey, but to do that track to gain the special skill set to be able to accomplish all these things while maintaining your own health is remarkable. I’m really grateful to be at this institution for what will be the next decade of my life in study and have the opportunity to see where it’s going to go in terms of research, becoming a center for patient care and a center for hope for hypermobility, essentially.
Christie:
Yeah, I’m a big believer in everything that’s happening at MUSC. They’ve been my surgeons and caregivers and I try to share all the great work the experts are doing at the Norris Lab. But I know one of the things that’s really challenging for them and must be for you, is despite the energy gained from being around this patient community and moving the ball forward, it’s also got to be really exhausting. I mean, you’re trying to go through 10 years of school, they’re trying to raise funds, they’re trying to change the world, one patient at a time. How are all of you getting this done?
Roman:
Yeah. It is hard. And the fact that nobody is doing it to this caliber anywhere else, it’s observing a one-of-a-kind thing being done for the first time that has so much potential to establish the legitimacy of this condition. I think a lot of people don’t realize people still get told ‘it’s all in their head.’ How do we make EDS more known? That’s done in the medical community through evidence-based research and education. That is a long-term thing that does not happen overnight. We can try our best to make a difference in the lives of individual people for now. What excites me about a career in medicine is that you do have that deep human interaction. And then consider the chain reaction and the ripple effect of that. A lot of this community impact is done at a grassroots level.
There are organizations that rally us together and bring us together, but a lot of us meet and we get information through online support groups, podcasts, and through our own experience, or books, where we have such deep, legitimate experience, and we get to pass that on. But that really shouldn’t be our job. It’s exhausting and it takes special people to do that. It’s amazing to see what’s being done here at MUSC so fast already. EDS in much greater detail is being added to the medical student curriculum at MUSC. It’s something that I never expected to happen— and how to see all these changes begin. It’s long overdue with EDS being discovered centuries ago. We need to spread the network. This teaching can’t just be at one place, one lab or one school of medicine, one hospital system—it has to be nationwide. That’s where I think the importance of this is.
It’s difficult because a lot of these conditions can be so debilitating, and sometimes we must put school on hold or maybe drop out to recover or care for ourselves. There are a lot of barriers. But who isn’t a better person to lead the charge against this than the people who have it, who are inspired, and interested—who have the personal experience to ask the questions that maybe no one else is asking or to think in that way because we live with this and understand how these things are connected? We think in a way that the typical medical education might not encourage you to think. Med school is a lot of memorization. It’s a lot of facts and there’s a lot of material. Fortunately, at MUSC, the way that they’ve been teaching future doctors definitely involves how to think outside the box—that each patient is unique. It is amazing because as a patient myself, I want to be treated the way that I’m being taught how to treat patients.
Christie:
Share with us details about your dual MD/PhD program that you’re going through at MUSC.
Roman:
Well, my primary career goal is to be involved in translational research. The big descriptive buzzword for that is the ‘bench to bedside approach.’ It’s an exploding field where the research directly informs care. There is a direct track where the researcher is also the one who may be generating the treatment or taking care of the patient. In a situation like EDS, where there are a lot of unknowns, I think it’s so important that the person who’s taking care of these people is up to date – really living on that cutting edge. Generating that knowledge and having that evidence-based track, having the ability to enroll patients in clinical trials—really to have an active hand in the clinical and the scientific space. Typically, if your job isn’t research, you’re seeing patients. And if you’re seeing patients, you don’t have time or the resources to do that basic science research. Luckily, I’ve met MD/PhDs here who graduated from the same program, running their own labs and still having clinic days.
Christie:
And one of the things that you know firsthand is that hypermobile EDS is more commonly diagnosed in females.Tell me, what’s your perspective as a male in this community with this diagnosis?
Roman:
The people in my family who are affected are all women—primarily my mom and sister. When I was diagnosed, the response was “Keep your fingers crossed. Even though you have the hypermobility and the family history, you probably aren’t going to develop anything serious since you’re a male.” The opposite happened. For most of my experience as a patient, I have been the only male in the room that was affected— I had EDS and had severe conditions derived from it. Currently, there’s a lot of talk about the sex difference and the degrees of presentation in hEDS. Like many experts, I wonder if there could be a hormonal aspect at play, where estrogen and testosterone have a role to play in the mitigation or worsening of EDS. Something is there for sure, but there are a lot of other unknowns. We live in a healthcare system where there are a lot of disparities. HEDS often gets labeled as a ‘hypochondriac white woman’s disease.’ That in many ways hurts a lot of people who are trying to get diagnosed for various reasons. A Person of Color with clear signs of EDS may be less likely to be diagnosed because the majority of those diagnosed are of European descent. A man may be assumed to be a much less severe case because it is typically women who are documented to present with severe comorbidities.
I remember growing up seeing my mom not being taken seriously in appointments, but if my dad was in the room, they were much more likely to believe things if he spoke on our behalf. It’s a shame, but it is true there’s a gender bias in healthcare, alongside other implicit and explicit biases toward other factors. We already have that issue in medicine and so many women encounter that specific barrier— then you consider the disparities involving access to care and the quality of that care. Previous literature on EDS says that it can affect all genders and ethnic backgrounds equally. Even though people of European descent are the ones diagnosed most often, that does not mean that people of other descent don’t have it. We see that hypermobility exists everywhere.
I’ve been told that it is “rare” to be a male with hEDS, but is it though? I’m not really sure. That’s something that we need to figure out. Somewhere between 70 to 80% of diagnosed cases are white women, who are between the teenage years to early to middle age— because of that 14-year time to get diagnosed after the onset of symptoms. Even though it’s the majority population being diagnosed, it doesn’t mean that there are other populations living with it— just not being diagnosed for varying reasons.
Christie:
There are so many questions today, but there are people like you that are turning to nursing or science, or medicine, or advocacy, or whatever they can do to be able to pick up the torch, and trailblaze this forward. Sometimes people at the beginning of a movement face challenges, and a heavy burden. But there’s a great deal of hope, and advancements that are coming. So, with your knowledge about medicine and research, what do you hope to be the future for hypermobile EDS? I personally would love to imagine a world where you took your child to your pediatrician, and maybe they had a symptom, or they noticed some level of hypermobility. Then simply they would run available diagnostic or genetic tests, like they do for a million other things, and you get a result back easily from a blood test. Then you can modify your child’s lifestyle and make accommodations to do the things you need to do to set your child up for success in life. Not to spend years figuring it out while you’re unraveling by that point, that you spend the rest of your life trying to make up for it. What’s your big hope for what’s going to happen in the medical and scientific community with hypermobility?
Roman:
I think that was a fantastic introduction. That’s a lot of the same stuff that I dream of. I know, just growing up, going through high school and going through college, I was really fortunate to get the right kind of care—but that was a lot in part because other people in my family had been through it and knew who to go to and how to work within the system. We were fortunate to have insurance and lived in somewhat close proximity to a lot of the expert physicians. What if I lived out somewhere like Iowa, for example, and I needed to travel to the DC/Maryland area to see all my specialists? How much money that must be—and if I had to work or take care of a family and be out of commission for months to recover from invasive surgery. Is that even possible? I’m very fortunate for my experience and my family’s support, which I know not everyone has in this community.
I think the body of future physicians and the kind of education that we’re receiving is priming us to consider all these other factors. This should hopefully make us a little bit more empathetic and a little bit more aware. And maybe more willing to break down some of these barriers I’ve mentioned now because we know that they exist. I’m going to be involved in research, I’m going to continue being involved in advocacy, education, the patient community, and in academia. I want to take this from beyond just a grassroots movement to an institutional movement— something similar to when a big discovery about cancer comes out. People follow that in droves and then replicate experiments, and they use it to move on and find new paths. I really hope that the great work a lot of the experts are doing right now will legitimize this disorder, so that we can have a future where a child comes into the clinic and their primary care observes they are outside the norm and suggests running a genetic test and making a game plan. This is in comparison to the typical “Oh, EDS? Maybe I know what that is, but I don’t know how to help you.” If we could have that in place – a broader understanding of EDS. Then we can have that protocol and a standard of care. I think if we live in this world where we know the complex genetics, than this can one day lead to medicinal treatments— not just surgical ones. We need to have it where everyone recognizes the name of this disorder as they do for other common diseases. Dr Norris calls it “the most common disorder you’ve probably never heard of.”
Christie:
Yes, to be in a position where there’s better diagnostic tools and there’s better treatment protocols. So that patients aren’t alone out there searching for answers, trying to get lucky finding that rare provider who understands. We’re grateful for your time and energy and appreciate you pausing during exam week and med school to join us. Kudos to your family and your parents, Pam and Steve, who have worked so hard to care for you and your sister, and have done so much for so many in advocacy and all the support groups, and all the things that they do to try to bring light to people that feel lost in the dark. Is there any other kind of message or piece of advice you’d like to give to patients, or other fellow medical students before we wrap up?
Roman:
Yeah, certainly, thank you for the kind words, it means so much to be able to be here and give my perspective and offer a glimmer of hope. We all are here to help each other. So, until we can edit somebody’s genome and just correct the mutations, it’s still going to be a lot. Until we get to that point, it is on patients to help other patients. I think it’s special how everybody’s EDS experience is so different, but also so relatable. I might meet someone who’s 20 years older than me and has a totally different life experience, but we can relate in so many ways. We can rely on each other, and we feel an obligation to want to help other people because we know what it is like. EDS can be really isolating, even if you have a great support system. For many patients, the people around you don’t really understand what you go through every day. People in your family who’ve known you your entire life have no idea what you deal with daily because you mask it and you push on. We have this unique experience and provide hope through community in whatever ways we can while remaining grateful and fighting for answers. There’s a lot of growth that can happen if you see it that way. It doesn’t mean you have to be a physician or a scientist. By sharing your story, you’re spreading hope, and you’re helping support this grassroots groundwork. It’s the idea that maybe in the future, when everything is better understood, no matter how big or small your role was, you did still play a role regardless. Because this is a community-based disease, it takes a village, and we help each other out.
Christie:
I’m a big believer in that. I always use the pun of it’s a “joint effort.” We’re all working together as patients helping patients, while we’re waiting for the medical community to get caught up. There’s a lot to being compassionate and empathetic towards other people. You’re an inspiration Roman and I’m so happy that you could join us here today. Keep us posted on your medical career. I’m looking forward to hearing from Dr. Fenner in the future.