How to be prepared & stay safe when having a hospital stay with Ehlers-Danlos syndrome (EDS)
This article will give an overview of ways you can prepare for a hospital stay when you have EDS, as well as tips on surgical prep and your own patient advocacy.
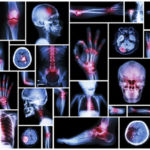
People with Ehlers-Danlos syndrome (EDS) often need surgery to fix joint problems, broken bones, or hernias. However, such procedures can be problematic for some. There are considerations to be aware of if you have EDS and a planned surgery.
First, EDS affects the connective tissues that provide structure to joints, skin, blood vessels, and other tissues and organs all over the body. The end results of this genetic defect is joint hypermobility and instability, skin texture anomalies, and vascular and soft tissue fragility. This can make it challenging for an untrained medical professional to know how to care properly for you. Be your own best advocate and learn how to help them help you. It can be quite overwhelming trying to stay safe and to know what to do when facing a hospital stay. Your best defense is to learn more and take a few steps to feel more in control and ensure your experience is as pleasant and safe as possible. With the proper preparation, you can be better informed and have the resources needed to make your hospital experience smoother.
[Disclaimer: The EDS Awareness Chronic Pain Partners media team has collected several resources in this article to guide you. Please refer to the citations in the sources below and to your doctor/surgeon for medical advice. This is not medical advice but a summation of published research and tips from patients shared for your use without obligation or responsibility.]
Basics to Know
Because of possible complications, you should only consider surgery as a last resort and at a surgeon’s advice. Consider getting second and even third opinions to ensure you make the right decision (as long as the situation is not an emergency). Common complications with EDS and surgery include excessive bleeding, wound healing problems, blood vessel tears, and concerns with anesthesia and other medications. More severe subtypes of EDS, including vascular conditions with fragile blood vessels, can be associated with higher rates of complications. Optimal treatment starts with a surgeon who has EDS knowledge and experience or at least is willing to learn and listen. Ask for a medical team familiar with your risks and needs for the best possible outcomes. Don’t be afraid to advocate for yourself but remember not to frighten off your doctors either. Understand that some complications cannot be prevented despite the best efforts, and let your medical team know that you and they are on the same side.
Prepare for What You Can Control
EDS patients should understand the risks of surgical complications and common difficulties around prolonged wound healing and scar tissue formation around the surgical site. Other issues can arise from comorbidities such as POTS, mast cell activation spectrum disorders (anaphylaxis, allergies to medications), and complex pain. Be sure to inquire with your doctors about their recommended wound bandages, medical tapes, or suture solutions for at home during the recovery period, with clear expectations on cleaning the wound. Also, discuss your options for pain management, nutritional needs, exercise or any physical limitations or restrictions post-op, like lifting or bending, and stooping.
Here are a few things that you can do before your surgery and hospital stay to better prepare:
- Prepare if you can in advance of any surgery or hospital stay by developing an emergency plan document and prepare for any potential emergency responders to better assist you as an EDS patient by checking out this article with links to resources on how to create a plan, get a medical ID, and share your medical binder with EMTs here.
- Always alert your surgical team in advance that you have Ehlers-Danlos Syndrome (EDS) and any comorbidities.
- Print out this journal article and give it to your surgeon for the discussion.
- Hydrate consistently for a few days before the procedure (in addition to any pre-op instructions you receive from your doctors) and consider drinking high-protein shakes to ensure your body is well nourished for 2-5 days prior.
- Warn your surgeon of any of your joints that tend to sublux most frequently, as they are more likely to do so when under general anesthesia.
- Have a loved one also advocate on your behalf by speaking directly (over and over if necessary) with each changing nurse crew, emphasizing the importance of any anaphylaxis reaction you may have and how to call for help in an urgency (including hitting the Code Blue button on the wall). MCAS patients can be fatally allergic to typical hospital products like rubbing alcohol, iodine, etc.
- Pack for comfort using the suggested list below for what to bring with you for your hospital stay to enhance the likelihood of successful outcomes and a more pleasant stay.
Here are a few essential tips and reprinted publication summaries to share with your doctor and /or surgeon to help prevent complications:
- Be aware EDS patients might need more local anesthetic and more general anesthesia.
- EDS patients have a higher rate of medication allergies, sometimes related to mast cell disorders.
- Consider an echocardiogram before surgery to check for any possible issues with blood vessels and the heart (aneurysms, valve prolapses or arrhythmias).
- Avoid extreme/prolonged patient positioning and over-stretching of tendons and ligaments already hypermobile.
- Be aware that rib subluxations are possible, and be cautious not to hyperinflate lungs.
- Consider closing wounds with subcuticular stitches and using adhesive dressings, which should remain on longer than usual to improve the healing process. Also, consider using a suture/adhesive strips combination technique for skin closure or recommend options for home use of Steri-strips (available to patients on Amazon) to close wounds beyond stitches and hold the wound closed longer.
- Avoid intramuscular injections because they can cause excessive bruising.
- Care should be taken not to cause injury to or dislocation of joints when elevating your limbs or moving your jaw for intubation; many patients have TMJ, hypermobile jaws and bruxism or clenching, all of which can make for more difficult intubation and post-surgical jaw complications.
- Try to avoid fluoroquinolone antibiotics if possible due to their risk of damaging connective tissue further.
- Have a medical alert bracelet made and wear these valuable identifiers to assist medical teams and emergency care responders with your care.
- Request all team hospital members, including PACU and ward floor nurses, know of the patient’s unique needs in advance for optimal patient care postoperatively and that printed signs are on their chart, posted prominently on wall signs, and printed and posted clearly on the patient’s hospital room door.
Complications to Watch for During Hospital Stays with Hypermobile EDS
Anesthesia:
- Local anesthesia might not work, or the patient might have a reaction to it (MCAS).
- Epidural anesthesia may cause CSF leaks, which might not heal quickly or completely in EDS patients.
Blood Vessels:
- Especially for people with vascular EDS, even minor surgeries can cause ruptures of blood vessels and increased bleeding or hematoma. Invasive monitoring, such as central venous catheters and treatment, should be avoided as much as possible.
Positioning during surgery:
- Incorrect positioning can lead to nerve compression and damage, skin injury, or joint dislocations; shear forces should be avoided, and joints could be supported by cushions.
Intubation:
- Intubation can lead to damage to the jaw, especially for people with TMJ.
- Intubation can worsen cervical spine instability or even cause it.
- Intubation can cause injuries to the trachea. This can be avoided using a smaller tube and fiberoptic techniques.
Skin and wound healing:
- Many people with EDS have slow or compromised wound healing. Sutures may have to stay in for longer.
- Bleeding: Some EDS patients have increased bleeding, which can cause massive blood loss during major surgery. In some cases, medication to improve blood clotting can be considered.
Postoperative complications:
- Hematomas
- Muscle weakness
- Deconditioning
Special measures in case of autonomic neuropathy:
- Monitor blood pressure fluctuations: Blood pressure and heart rate can fluctuate dramatically in these patients, significantly when changing their position. Long periods of hypotension can occur during surgery.
- Fast re-conditioning after surgery
- Caution with certain medications that could potentially worsen dysautonomia, for instance, vasodilators, narcotics, nortriptyline, amitriptyline, antidepressants, epinephrine (which may be needed in case of MCAS reaction), thiopental, or ketamine.
- Monitor temperature fluctuations
- Avoid dehydration
Special measures in case of MCAS
- Minimize stress because physical and mental stress can trigger reactions; this also includes stressors during surgery, like blood loss, hypothermia, adrenal insufficiency, and various drugs. Surgical techniques that cause the smallest trauma should be preferred.
- Check coagulation status before surgery.
- Give preventive medication before surgery (such as H1 blockers, H2 blockers, corticosteroids, Vitamin C)
- Be prepared for emergencies and have emergency meds ready to use (like adrenalin)
- Strict monitoring after surgery: for allergic reactions but also blood clotting issues (both ways: bleeding but also thromboses are possible).
Special measures in case of CCI
- Adapt intubation method: For instance, fiberoptic intubation may be preferred, so the neck doesn’t have to be hyperextended as much.
- Strict monitoring during surgery to evaluate possible spinal cord damage.
Potential Surgical Risks in Patients with Ehlers-Danlos Syndrome
- Damage to an unstable cervical spine
- TMJ dislocation/subluxation
- Neurologic injury/compression
- Damage secondary to Occipital Atlantoaxial instability, cervical instability (consider pre-op cervical flexion and extension x-rays)
- Damage to Fragile mucosa/skin
- Lung injury/pneumothorax/shunt
- Increased risk of ocular injury
- Vascular damage
- Intestinal rupture
- Increased risk of poor wound healing
- Increased risk of hypotension/orthostasis secondary to dysautonomia (POTS), may need aggressive IV fluid use.
- More-than-expected postoperative pain; Aggressive pain management is recommended and be aware opiates may not be effective; consider a high dose of Tylenol, Tramadol, and neuropathic agents.
- Allergic reactions are common due to mast cell dysfunction; consider pre-treatment with antihistamines, steroids and/or benzodiazepines.
- Gastroparesis can result; aggressively use laxatives.
Patient Pack List for a Hospital Stay
- Copy of your identification, medical insurance info, pharmacy info, primary doctor info, allergy info
- Current medication list with times taken so it can be cross-referenced with RX given during stay by hospital
- Toiletries for bathing, disposable toothbrushes
- Lip balm, lotion, and baby powder
- Hairbrush/comb, hair ties or clips, dry shampoo spray
- Antiseptic wipes, make-up remover face wipes, baby wipes
- Gum or mints, lozenges, hard candies for dry mouth
- Supplies for eye contacts, glasses, eye drops
- Comfy pajamas, preferably button-down style or wide neck opening for ease of pullover
- Slip-on shoes vs. lace-up, skid-proof slippers or socks.
- Soft knit hat for warmth, extra blanket
- Notepad, pen, and paper for when it’s hard to talk or take notes with memory issues
- Contact list with phone numbers of those to call with updates
- Side sleeper pillow or a U-shaped pillow (sanitize it beforehand by washing your pillow with 1 cup powdered dishwashing detergent and 1 cup bleach in warm water)
- Magazines, books, tablet, headphones for entertainment
- Cellphone, chargers, and battery backups
- Cash for vending machines
- Snacks for yourself, visiting loved ones, or the nurses
- List of questions ready to ask during discharge (Physical therapy, follow-up appointment, etc.)
Need More Help?
If you need help explaining your needs to your provider, consider hiring an EDS-aware patient advocate or order an informative pamphlet to give to your doctor or surgeon created by well-known EDS non-profit resources here https://www.redcliffhousepublications.co.uk/product-page/preoperative-assessment-guidance-heds-hsd
Bottom Line: Mistakes Happen in Hospitals, and Caregivers are Overburdened by the System, so Take Charge of Your Own Health and Safety by Being Prepared
Directly from physician research articles below sums it up well…
“With a wide array of medical complications requiring frequent physician-patient interactions for individuals with hEDS, patient hesitancy to describe all their symptoms may form. Diffuse joint pain, head and spine pain, sensory overwhelm, POTS, gastroparesis, and other symptoms associated with EDS must be kept in mind when treating patients. With a wide array of medical complications requiring frequent physician-patient interactions for individuals with EDS, patient hesitancy to describe all their symptoms may form. Patients may show apprehension or nervousness in discussing their symptoms, which often results in diagnoses of anxiety, depression, and fibromyalgia. However, rather than having primary psychiatric or rheumatologic disorders, these patients are instead in a state of dysautonomia, and may also have post-traumatic stress from repeated medical complications. Therefore, physicians should take the initiative to understand these correlations to proactively prevent unnecessary complications for patients during their hospital course.”
Source: Clarke, J.E., Santana, J. and Manjarrez, E.C., 2022. Hospital Stay Considerations in Hypermobile Ehlers-Danlos Syndrome: An Exemplary Case With Insights for Coexisting Symptoms. Annals of Internal Medicine: Clinical Cases, 1(4), p.e220154.
You can download this article as an e-book:
Surgery Prep: Meeting Your EDS Hospital Stay Needs
You might also find this article interesting:
Basic Emergency Care Planning for EDS Patients
Curated by Chronic Pain Partners Media Team & medically reviewed by an expert.
March 2023
Sources used in this article and more information:
Wiesmann, T., Castori, M., Malfait, F. and Wulf, H., 2014. Recommendations for anesthesia and perioperative management in patients with Ehlers-Danlos syndrome (s). Orphanet Journal of Rare Diseases, 9(1), pp.1-9.
Clarke, J.E., Santana, J. and Manjarrez, E.C., 2022. Hospital Stay Considerations in Hypermobile Ehlers-Danlos Syndrome: An Exemplary Case With Insights for Coexisting Symptoms. Annals of Internal Medicine: Clinical Cases, 1(4), p.e220154.
Prepare for Surgery – Tulane Hypermobility Clinic: https://hypermobilityclinic.org/surgical-and-anesthetic-precautions-for-hypermobile-and-eds-patients/
Søborg, M.L.K., Leganger, J., Rosenberg, J. and Burcharth, J., 2017. Increased need for gastrointestinal surgery and increased risk of surgery-related complications in patients with Ehlers-Danlos syndrome: a systematic review. Digestive surgery, 34(2), pp.161-170.
https://www.karger.com/Article/Fulltext/449106
Preoperative assessment guidance – hEDS & HSD: https://www.redcliffhousepublications.co.uk/product-page/preoperative-assessment-guidance-heds-hsd
Precautions to Consider Before Surgery When You Have EDS:
Chapuis, H., Peyrolade, A., Féki, A., Clauss, F. and Bornert, F., 2020. Surgical-orthodontic treatment in patients with Ehlers–Danlos syndrome: a report of two familial cases. Journal of Oral Medicine and Oral Surgery, 26(1).
Brooke, B.S., Arnaoutakis, G., McDonnell, N.B. and Black III, J.H., 2010. Contemporary management of vascular complications associated with Ehlers-Danlos syndrome. Journal of vascular surgery, 51(1), pp.131-139.
Orthopaedic surgery in hypermobile Ehlers-Danlos syndrome and Hypermobility Spectrum Disorders: https://www.ehlers-danlos.org/information/orthopaedic-surgery-in-hypermobile-ehlers-danlos-syndrome-and-hypermobility-spectrum-disorders
Beighton, P.H. and Horan, F., 1969. Orthopaedic aspects of the Ehlers. Danlos syndrome. The Journal of bone and joint surgery. British volume, 51(3), pp.444-453.
Pepin, M., Schwarze, U., Superti-Furga, A. and Byers, P.H., 2000. Clinical and genetic features of Ehlers–Danlos syndrome type IV, the vascular type. New England Journal of Medicine, 342(10), pp.673-680.
Information for Potential Patients – Baylor College of Medicine: https://www.bcm.edu/healthcare/specialties/medical-genetics/for-patients
Boston University research: Exploring medical comorbidities and surgical history of individuals presenting with hypermobile Ehlers-Danlos syndrome: a retrospective chart review:
https://open.bu.edu/handle/2144/45542
Clapp, I.M., Paul, K.M., Beck, E.C. and Nho, SJ, 2021. Hypermobile disorders and their effects on the hip joint. Frontiers in surgery, 8, p.596971.
Kroese, L.F., Mommers, E.H., Robbens, C., Bouvy, N.D., Lange, J.F. and Berrevoet, F., 2018. Complications and recurrence rates of patients with Ehlers-Danlos syndrome undergoing ventral hernioplasty: a case series. Hernia, 22, pp.611-616.
Lohkamp, L.N., Marathe, N. and Fehlings, M.G., 2022. Craniocervical instability in Ehlers-Danlos syndrome—A systematic review of diagnostic and surgical treatment criteria. Global Spine Journal, 12(8), pp.1862-1871.
Clarke, J.E., Santana, J. and Manjarrez, E.C., 2022. Hospital Stay Considerations in Hypermobile Ehlers-Danlos Syndrome: An Exemplary Case With Insights for Coexisting Symptoms. Annals of Internal Medicine: Clinical Cases, 1(4), p.e220154.
Ericson Jr, W.B. and Wolman, R., 2017, March. Orthopaedic management of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 188-194).
Waller, D.G. ed., 2016. Rheumatology and Autoimmune Rheumatic Disorders E-Book: Prepare for the MRCP: Key Articles from the Medicine journal. Elsevier Health Sciences.
Koch, K., 2020. EMS Response to Patients with Special Needs: Assessment, Treatment and Transport. Fire Engineering Books.
Knight, I., 2013. A Multidisciplinary Approach to Managing Ehlers-Danlos (type III)-Hypermobility Syndrome: Working with the Chronic Complex Patient. Singing Dragon.
Guide for patients who have surgery:
https://me-pedia.org/wiki/Guide_for_patients_having_surgery
Wendy 4 Therapy website:
https://www.wendy4therapy.com/surgical-consideration-for-patients-with-eds
Mustafa, H.I., Fessel, J.P., Barwise, J., Shannon, J.R., Raj, S.R., Diedrich, A., Biaggioni, I., Robertson, D. and Warner, D.S., 2012. Dysautonomia: perioperative implications. The Journal of the American Society of Anesthesiologists, 116(1), pp.205-215.
Sido, B., Dumoulin, F.L., Homann, J., Hertfelder, H.J., Bollmann, M. and Molderings, G.J., 2014. Chirurgische Eingriffe an Patienten mit Mastzellüberaktivitätserkrankung. Der Chirurg, 85(4), pp.327-333.
Schievink, W.I. and Deline, CR, 2014. Headache secondary to intracranial hypotension. Current pain and headache reports, 18(11), p.457.
Schievink, W.I., Gordon, O.K. and Tourje, J., 2004. Connective tissue disorders with spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension: a prospective study. Neurosurgery, 54(1), pp.65-71.
Johnston, B.A., Occhipinti, K.E., Baluch, A. and Kaye, A.D., 2006. Ehlers-Danlos syndrome: complications and solutions concerning anesthetic management. Middle East journal of anesthesiology, 18(6), p.1171.
Tinkle, B.T., 2010. Joint hypermobility handbook: A guide for the issues & management of Ehlers-Danlos syndrome hypermobility type and the hypermobility syndrome. Greens Fork, Indiana: Left Paw Press.
Nakagawa, H., Wada, H., Hajiro, T., Nagao, T., Ogawa, E., Hatamochi, A., Tanaka, T. and Nakano, Y., 2015. Ehlers-Danlos syndrome type IV with bilateral pneumothorax. Internal Medicine, 54(24), pp.3181-3184.
Lindsay, H., Lee-Kim, Y.J. and Srivaths, L.V., 2016. Perioperative hemostatic management in Ehlers-Danlos syndrome: A report of 2 cases and literature review. Journal of pediatric hematology/oncology, 38(2), pp.158-160.
Paepe, A.D. and Malfait, F., 2004. Bleeding and bruising in patients with Ehlers–Danlos syndrome and other collagen vascular disorders. British journal of haematology, 127(5), pp.491-500.
Petersen, W. and Laprell, H., 1998. The “insidious” rupture of the achilles tendon after ciprofloxacin induced tendinopathy. A case report. Der Unfallchirurg, 101(9), pp.731-734.
Le Huec, J.C., Schaeverbeke, T., Chauveaux, D., Rivel, J., Dehais, J. and Le Rebeller, A., 1995. Epicondylitis after treatment with fluoroquinolone antibiotics. The Journal of bone and joint surgery. British volume, 77(2), pp.293-295.
Rabbitts, J.A., Groenewald, C.B., Jacob, A.K., Low, P.A. and Curry, T.B., 2011. Postural orthostatic tachycardia syndrome and general anesthesia: a series of 13 cases. Journal of clinical anesthesia, 23(5), pp.384-392.
Corbett, W.L., Reiter, C.M., Schultz, J.R., Kanter, R.J. and Habib, A.S., 2006. Anaesthetic management of a parturient with the postural orthostatic tachycardia syndrome: a case report. BJA: British Journal of Anaesthesia, 97(2), pp.196-199.
Molderings, G.J., Homann, J., Brettner, S., Raithel, M. and Frieling, T., 2014. Systemische Mastzellaktivierungserkrankung: Ein praxisorientierter Leitfaden zu Diagnostik und Therapie. DMW-Deutsche Medizinische Wochenschrift, 139(30), pp.1523-1538.
Raithel, M., Huber, H., Malteser WKH Erlangen, 2021. Interventionelle Eingriffe, Anleitung für Patienten mit Mastzellerkrankungen. VAEM e. V.
Yaszemski, M.J. and Shepler, T.R., 1990. Sudden death from cord compression associated with atlanto-axial instability in rheumatoid arthritis. A case report. Spine, 15(4), pp.338-341.
Edge, C.J., Hyman, N., Addy, V., Anslow, P., Kearns, C., Stacey, R. and Waldmann, C., 2002. Posterior spinal ligament rupture associated with laryngeal mask insertion in a patient with undisclosed unstable cervical spine. British journal of anaesthesia, 89(3), pp.514-517.
Al Bahri, R.S., MacDonald, D.B. and Mahmoud, A.H.M., 2017. Motor and somatosensory evoked potential spinal cord monitoring during intubation and neck extension for thyroidectomy in a Down syndrome boy with atlantoaxial instability. Journal of clinical monitoring and computing, 31(1), pp.231-233.
Louie A, Meyerle C, Francomano C, Srikumaran D, Merali F, Doyle JJ, Bower K, Bloom L, Boland MV, Mahoney N, Daoud Y, Singman EL. Survey of Ehlers-Danlos Patients’ ophthalmic surgery experiences. Mol Genet Genomic Med. 2020 Apr;8(4):e1155. doi: 10.1002/mgg3.1155. Epub 2020 Jan 27. PMID: 31989797; PMCID: PMC7196452.