The EDS & Aging Project
Funny Bone Newsletter – March 2022
presented by EDS Awareness
This is a community-centered project with people older than 45 who want to share their experiences about aging as a person with EDS. This project will be published as part of the EDS Awareness Newsletter in a collaboration between CEO John Ferman and journalist Karina Sturm.
For a more appealing presentation of this project,
Click HERE
Foreword
The Funny Bone News came to life when John, CEO of EDS Awareness, asked me if I, as a journalist, would want to lead a new community-focused project: a newsletter that shares news, research, and valuable content for our community. How could I have said no to it? So almost a year ago, we sent out our first newsletter, and since then, a lot has happened. We received many responses from you, our readers, mentioning various topics they would be curious to learn more about. So every month, I spend several hours curating the newsletter, including whatever you asked me to feature.
A while ago, a community member reached out and told us about the lack of support for aging people with EDS. Now, I am 35 and didn’t have too much exposure to this subject, but I quickly realized that a lot of the information on EDS is tailored to a younger community or people newly diagnosed with EDS, but I couldn’t find much specifically supporting older EDSers. EDS Awareness decided it was time to change this, and the EDS & Aging Project was born.
This being said, in the future, we plan more projects like this focusing on other aspects of life with EDS. For example, we would love to hear from our male community as well, but one area I am particularly interested in is to feature people who belong to multiply marginalized communities! If you feel like this is you, please get in touch, and let’s work together!
Cheers,
Karina
- Introduction
You – the people within our community – all know the Ehlers-Danlos syndromes are a diverse spectrum of conditions. Not only does every type come with its specific set of features, but even within one and the same type, symptoms can vary from mild to very severe. People can have almost no limitations throughout daily life; others might identify as being disabled.
However, one area that’s barely ever talked about is: EDS & Aging. Why is that? I mean, we apparently all grow older. It is well documented in the literature that symptoms of EDS might be tied to hormonal fluctuations. For example, many people with EDS describe experiencing a progression of EDS symptoms with puberty; others say, when they got pregnant, their condition changed; and then there is menopause, which marks another milestone in everyone’s, but especially an EDSers life.
So with this project, we wanted to give a voice to the aging EDS population. We asked them each five questions, and here, we present to you a selection of their responses, which will hopefully support other aging people in the community or lead the way for people in their 30s or 40s who really don’t know what to expect in the future.
- Meet the Participants
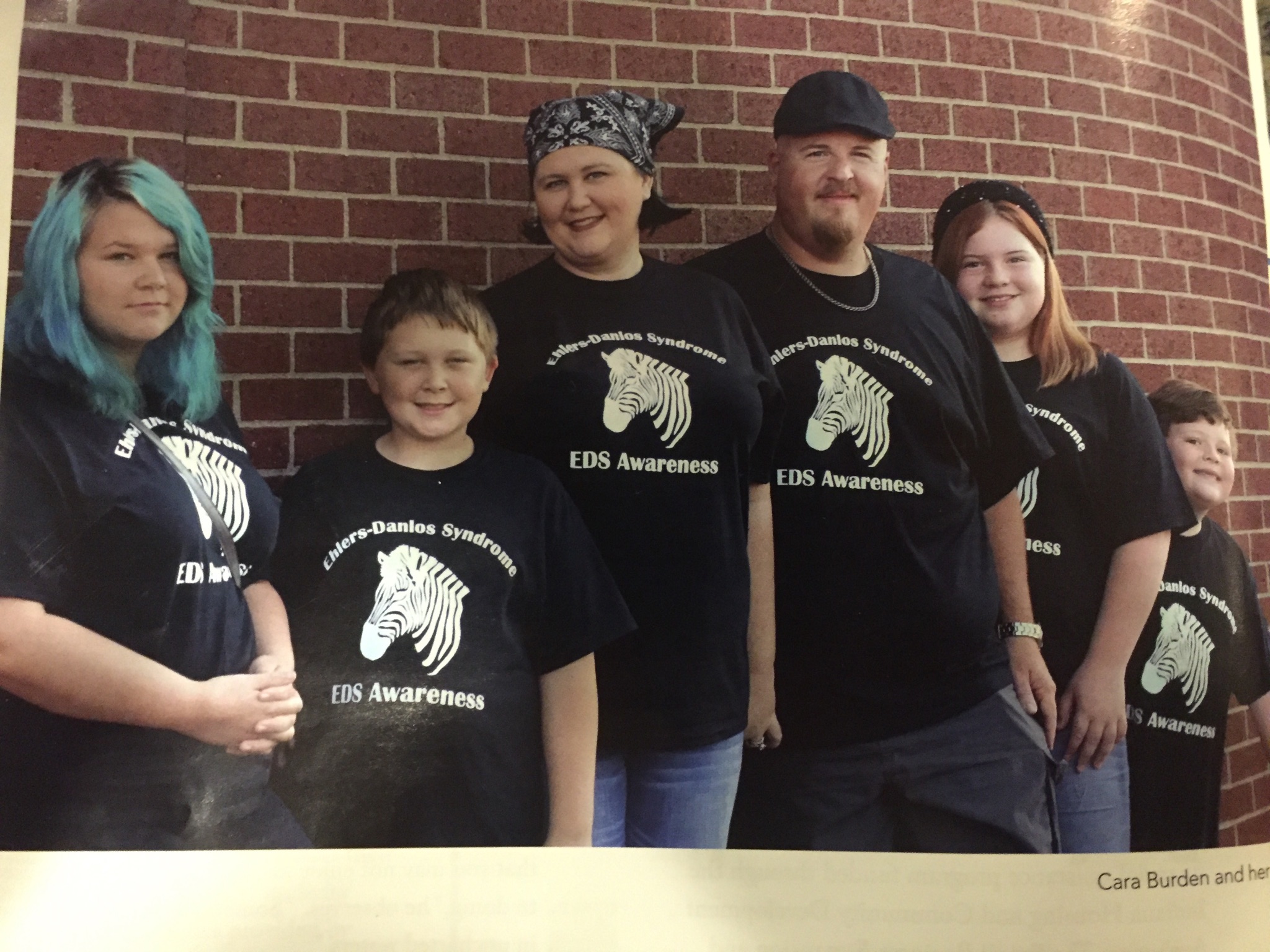
Images of all participants can be found in the PRESENTATION
(We asked via Social Media for people who wanted to contribute and included every person that got in touch with us!)
Jennifer A.: Jennifer is 62 years old, lives in England, UK, and was diagnosed with hEDS, PoTs and MCAS.
Delia W.: Delia is 70 years old, lives in Maine, US, and was diagnosed with an undetermined variant of EDS.
Kathryn S.: Kathryn is 55 years old, lives in Washington, US, and was diagnosed with hEDS.
Karyn W.: Karyn is 55 years old, lives in Yorkshire, England, and was diagnosed with hEDS, MCAS, depression and chronic fatigue.
Susan E.: Susan is 53 years old, lives in Pennsylvania, US, and was diagnosed with hEDS/HSD.
Jeanne M.: Jeanne is 62 years old, lives in New York, US, and was diagnosed with cEDS.
Margaret E.: Margaret is 58 years old, lives in New York, US, and was diagnosed with hEDS.
Elizabeth M.: Elizabeth is 50 years old, lives in Florida and was diagnosed with EDS.
Ulrike M.*: Ulrike is 75 years old, lives in New York, US, and was diagnosed with hEDS.
Han de V.: Han is 67 years old, lives in the Netherlands and was diagnosed with hEDS.
Melissa M.: Melissa is in her 60s, lives in Arkansas, US, and was diagnosed with hEDS and vEDS.
Eve G.: Eve is 57 years old and was diagnosed with EDS.
Monica H.*: Monica is 60 years old, lives in Switzerland and was diagnosed with HSD.
Pashondra J.: Pashondra is 48 years old, lives in North Carolina, US, and was diagnosed with EDS.
Jon R.: Jon is 63 years old, lives in Massachusetts, US, and was diagnosed with Marfan syndrome and EDS.
Jim B.: Jim is 65 years old, lives in California, US, and was previously diagnosed with EDS but is now classified as Loeys-Dietz syndrome.
Wilder E.: Wilder is 54 years old, lives in Connecticut, US, and was diagnosed with hEDS, PoTS, MCAS and Gastroparesis.
Sonya G.: Sonya is 56 years old, lives in Pennsylvania, US, and was diagnosed with clEDS, MCAS and hyperadrenergic PoTS.
Isabel R.: Isabel is 48 years old, lives in Rhode Island, USA, and was diagnosed with hEDS.
*Name changed per request.
- Questions
We asked our participants five questions:
When you look back, how have your symptoms changed over time?
What’s the biggest challenge related to your age and EDS?
What needs to change for people your age in terms of EDS?
What do you wish your 25-year-old self would have known about aging with EDS?
What are the top five things that help you with your symptoms related to aging with EDS?
- Responses
(A selection of our participant’s responses.)
For a more appealing presentation of this project,
Question 1: When you look back, how have your symptoms changed over time?
“Despite hEDS, I was a competitive athlete, exercising most of my life. I developed long, lean muscles which protected my fragile tissues. I was able to receive an education, enjoy a career, fall in love and have a family. I lived a relatively normal life with chronic pain through my late 40s. As I’ve aged, my hEDS symptoms have progressively gotten worse. I’ve developed vascular complications that threatened my life twice. I am 58 and still hypermobile. Musculoskeletal pain, dislocations, and joint injuries have occurred throughout my life. I’ve suffered from anxiety, migraines, allergies, fragile skin, pelvic floor instability, easy bruising, Raynaud’s, gastrointestinal symptoms and autonomic dysfunction (PoTS). At 52 years old, everything changed when I suffered two cervical artery dissections: rare vascular complications related to EDS. I then learned I have an aortic aneurysm that is monitored frequently with heart scans to prevent another vascular complication.” – Margaret E.
“Yes, symptoms have changed over time, particularly increasing fatigue and recovery time from exertion that unaffected others take for granted.” – Jennifer A.
“Over time, my symptoms have become more severe. I’ve sustained a lot of loss. I used to be able to walk long distances, knit, play guitar, sing, swim for a mile, take ballet lessons, and engage in all sorts of activities. I’ve lost the ability to do all of the things I mentioned above, which, for a while, led to some isolation and loss of identity.” – Jeanne M.
“The symptoms were always there; I simply didn’t realize they were symptoms of EDS. For example, I thought everyone subluxed ribs when they laughed because my mom did too, and it was typical for our family (three generations of previously undiagnosed EDS). That said, as I’ve aged, my symptoms have worsened. I have increased pain, more frequent injuries, longer healing times, and more joint laxity.” – Kathryn S.
“The main symptom that has changed as I’ve got older is MCAS. I seem to collect more allergies and sensitivities with every passing year. I’ve also learned to be better at managing fatigue; I wish I could have learned those skills earlier.” – Karyn W.
“I’m in my sixties now. The older I get, the more elasticized my joints have become. When I was in my thirties, I could loosen a stuck jar lid. Now, if I try to do that, it will result in a sprained wrist. When I was in my thirties, my hip joint would slip out of place and become inflamed if I lifted something heavy. Now it will do that if I sleep on my side for too long. I sprained my shoulder a couple of years ago when I placed my arm on the side of the bathtub and pushed up to get out of the tub. That sort of ridiculously easy spraining never happened when I was younger. In addition, the older I get, the less effective local anesthesia has become until it now does not work at all. This has come up with dental work, needing skin biopsied, needing a thyroid piece biopsied, laser eye surgery on my retinas, etc. My dentist has to either use general anesthesia on me or no anesthesia at all. I’ve screamed in pain in medical facilities as they tried to do something after several local anesthesia shots. They act like I’m some crazy person who is being melodramatic. I hate not being believed, as I am actually a calm, logical person not given to emotional outbursts. I recently forewent having needed cataract surgery due to local anesthesia not working on me. This is an example of how sometimes we can’t get medical care (cataract surgery) that would be available to us if we did not have EDS.” – Melissa M.
“As I think back, I can see exactly when my symptoms started to get progressively worse: after my hysterectomy. I went from being tired to sheer exhaustion, and my little aches and pains turned into extremely debilitating pain, and everything hurts.” – Pashondra J.
“I wasn’t diagnosed at an early age, but once I was diagnosed in my 50s, it explained a lot of things that occurred when I was younger. Back in the 80s, I was very athletic; however, I had frequent injuries that were just attributed to sports. When thinking about how little is known among doctors about EDS today, you can imagine that EDS was not even on the radar back then. I was very flexible, but that was attributed to my sports training. However, in order to play, I also had to tightly tape wrap areas of my body, specifically feet and ankles, in order to have the support to play and avoid injury. No one thought that this was unusual then (schools didn’t have trainers on sidelines like they do today for injuries and concussion protocols), but again as I aged, it became clear that injuries that occurred were no longer sports-related. Something was very wrong as my body began to come apart in ways it never had before and with the simplest movement. I think one of the main differences I have as an older person with hEDS is that while being bendy, I’ve lost some of my bendiness/flexibility that naturally occurs with age. So my Beighton score is technically an eight, but realistically now is a six due only to aging (and my geneticist has noted this in my records).” – Wilder E.
Question 2: What’s the biggest challenge to your age and EDS?
“The criteria the majority of standard pain doctors use for EDS pain patients are fitted around a baseline for people without the disease, so EDS patients are treated as though their pain stems from only one area, similar to a long-term injury when in fact flares can happen throughout the body. So when you say another area is flaring, they look at patients like they are malingering. Another thing I find challenging is to get doctors to get past what they see. They think, “Oh, she looks fine; therefore, she is fine.” As I have gotten older, I realize that some medication and therapies that worked well early in my diagnosis no longer work, and some doctors don’t want to look into any further treatment because they don’t understand and then try to push us off on other doctors. It seems like a never-ending merry-go-round, and it’s frustrating. I also realize that the older I get, the more expensive my treatment gets, and that is with insurance.” – Pashondra J.
“I’m frustrated not being able to do everyday things I previously could (such as opening jars, cooking elaborate meals, writing, exercising, crafting with wool felt, photography, and working as a technical writer). Also, grappling with feelings of guilt that I’m a burden to my healthy, younger husband. The mental toll of being in near-constant pain affects most aspects of my life, particularly my sleep.” – Kathryn S.
“I live by the spoon theory. I have days when I can’t do much at all and days when I ‘catch up’ from the bad days. I’ve learned to say no and have adjusted my life to account for the days I can’t do anything. Cleaning, which took me four hours, now takes me all day, and I have my husband help me. I have days that I can’t even shower. I try to keep my life as simple as possible. In regards to health care providers, fortunately, EDS is becoming more well-known, and I find that the younger medical professionals are knowledgeable. I take printouts to my appointments from ehlers-danlos.com that explain possible issues related to my visit.” – Susan E.
“Comorbidities that became fully realized following a series of surgeries. Trying to get diagnosed with rare conditions in the middle of a pandemic has been difficult. At 70 docs still lean towards aging as opposed to actual rare conditions.” – Delia W.
“Health care providers, even those with some EDS knowledge, have little (or no) experience with patients of a certain age. My geneticist/cardiologist has said that she has only a few patients my age or older (and she is quite well known among the local EDS community). PT has to be adapted for the aging, fewer repetitions, gentler and perhaps different exercises. Family has been a huge challenge. Since being diagnosed three years ago, only one person in the family (and we are a close family) has looked up EDS and the comorbidities. My husband, approaching 90, has no idea at all – only that I am not able to care for him, go anywhere with him, etc. However, EDS and all the comorbidities and resulting traumas have had a devastating effect on him and his aging process as well. This, in turn, has caused another devastating effect on the whole family. I began needing a caregiver in August of 2019, after ileostomy surgery. Aside from the poor healthcare in the US, New York City is experiencing more and more doctors simply opting out of Medicare – leaving the elderly patient to bear the full, often exorbitant cost. In addition, there are so many things that are not considered medical necessities and thus not covered: supplements, legal medical marijuana, all types of splints, braces, cushions, ointments, pain patches. Often, one has no idea what may help and tries every possibility, often throwing them out as they are no help. This goes on and on in an effort to find relief! I recently had to hire a Health Care Advocate, as I became overwhelmed managing so many different doctors and caregiver vetting, at an exorbitant cost!” – Ulrike M.
“When you have been unable to work for 15 years, and you can’t go out with friends anymore, it leads to feelings of loneliness. That feeling makes me sad. You often have to look for the little things that bring you joy and get your emotional life back into balance. It can be done for sure, but it is hard work.” – Han de V.
“My biggest challenges right now are all related to being upright for over an hour. Driving places, sitting in chairs at family gatherings, sitting anywhere in a waiting room or at a restaurant are all tough! Friends are used to seeing me lay down in random places after a hike or bike. Heck, I lay down anywhere I can. Another challenge is that I have a super upbeat, positive personality and look extremely fit and ‘normal.’ Family, health care providers other than my ortho and PT, and people in general have absolutely NO idea what is going on inside my body. I prefer to remain positive and look fit instead of giving up!” – Eve G.
“The biggest challenge I face is avoiding falling into a state of depression. I’m constantly pushing myself to carry on, to fulfill my role as a wife, mother and caregiver. It’s exhausting. I feel like the pain I am in isn’t validated by anyone. It’s no point to mention it anymore as it’s not severe enough in the eyes of family, friends, coworkers and even my doctors. I often sublux even walking to the bus stop or while sleeping. I have to get up three hours before my shift starts to appropriately deal with how I might wake up. Nobody sees that, and emotionally, it drains you.” – Monica H.
“There are many challenges that I face, which are complicated by my age and the nature of my weakened/defective connective tissue. In regards to my health care providers, it is always important to balance what I need from my doctor and what I can actually say. New doctors are always an added challenge due to my age since aging issues tend to be blended in with my actual connective tissue degeneration. In regards to family, age has actually helped their understanding of what I have gone through because now they are going through some of the health challenges I have had my whole life, for example, bone and joint pain and fatigue. As I have aged, I have learned ways to deal with the ebb and flow of connective tissue issues. Having had to roll with punches and deal with the unexpected has made me more aware of what matters and doesn’t as I have aged.” – Jon R.
“The biggest challenge I have right now is that doing all the things I need to do to keep myself feeling my best is very time-consuming. Working on stability and strength, making time for movement, food preparation and restrictions is all very time–consuming.” – Isabel R.
Question 3: What needs to change for people your age in terms of EDS?
“No question it’s different at 70, and so much of the written literature is about and directed towards young people. We are rarely represented in the EDS community. I have warnings – they need to listen.” – Delia W.
“I’m fortunate that I have a well-paid part-time job, so I’ve paid privately for physiotherapy. If I weren’t in this privileged position, I wouldn’t have got the help I needed. This really needs to change so that everyone can access the support they need. Working part–time and working from home because of COVID have been game–changers for me. My quality of life is so much better because I have energy for things other than work and survival now. I’d love to see these opportunities become much more mainstream.” – Karyn W.
“In order for things to change for people my age, health care needs to be both accessible and affordable. High insurance premiums, high deductibles and high co-pays cause American health care to be unaffordable for most. After paying expensive premiums, there isn’t much left in the budget for costly prescriptions and treatments. Physical therapy, medications and scans are necessary to monitor fragile musculoskeletal and vascular tissues, yet co-pays are expensive and treatments limited annually.” – Margaret E.
“Our EDS community needs to get more comfortable with Disability. Many of us are Disabled, but we continue to judge ourselves, and we allow ‘abled’ society to set goals for us instead of setting them for ourselves. Members – leaders even – of our community present unrealistic examples of physical activity and ‘recovery’ that are not possible for many EDSers because of their symptom burden or their day-to-day responsibilities – or even because they choose to spend their limited energy in places other than the gym or PT. There are few opportunities for Disabled voices to be heard and celebrated.” – Jeanne M.
“We need doctors, PTs, dentists, eye docs who are well trained in EDS! There are literally NO docs in my area that have any clue other than a book definition. I tried to get disability, and because I was exercising, even though it was just an hour, they denied me. I am unable to do any job at all. I was working as an online teacher where I could lay down and teach, but then I got a concussion that ruined my vision, so even computer work was out. The judges do not understand EDS, nor do some of the doctors who are considered experts.” – Eve G.
“People of my age need more studies done, which will help medical professionals treat us. My issues have spread to my entire body. I can’t express how tired I am of hearing, ‘lose weight and strengthen your muscles.’ Twenty years ago, I was a single mother of two; I could beat men at arm wrestling, rode motorcycles, was a roller coaster enthusiast, AND you could eat off of my floors as my house was always clean… now I’m happy if I can shower, cook and clean.” – Susan E.
“We definitely need more research to hopefully find a cure and more ways to manage symptoms. It seems like what care we see is geared towards pediatric and geriatric patients. It would be nice to see support groups for patients that are middle-aged and having to transition to different jobs or leaving the workforce completely due to disability as I had to do.” – Pashondra J.
“I find many just want to blame EDS health issues on old age and not really look into viable solutions to help you. I guess when you are older, you are just supposed to live with it because that is what older people do. So I think in our society there needs to be a change in this attitude. Older people can get better with the correct therapies too.” – Jim B.
“Awareness needs to change, and it needs to stop that we call it a rare condition. We need more education in the medical community, including physical therapy, all medical modalities that are not necessarily considered conventional, and mental health support needs to improve, especially for people who are on the severe end of the spectrum.” – Isabel R.
“What needs to change, regardless of age, in terms of EDS is: More training and awareness across the medical field (doctors, nurses, therapists, dieticians, etc.); more access to testing and patient-focused healthcare (or testing regardless of health insurance); more research to find cures for EDS or in the meantime, more access to management of the disorder (and a consensus on the types of therapeutics to consider); more access to effective pain management without the stigma of being drug (opioid) chasers… and preferably plant medicine such as cannabis; more compassion for complex patients like those with EDS.” – Wilder E.
Question 4: What do you wish your 25-year-old self would have known about aging with EDS?
“My 25-year-old self had no idea EDS existed and /or that I had it. It would have been beneficial to know. Also, had it been taught in Medical school in those days and earlier, perhaps the gene for hEDS would have been identified long ago, and some actually helpful therapies created. As this was not the case, my 25–year–old continued to probably do everything wrong to make my 75–year–old self hurt and suffer more than might have been necessary?!” – Ulrike M.
“I wish my 25-year-old self had an hEDS diagnosis. I didn’t receive a diagnosis until I was 56, despite connective tissue symptoms from birth. I was blindsided at 52 when I suffered two cervical artery dissections despite a strong family history, including my dad’s sudden death at 52 and my older brother’s open heart repair, aged 52. My vascular connective tissue disease is considered a rare form of hEDS. Genetic testing on a comprehensive aortopathy panel was negative for vEDS. I met the clinical diagnostic criteria for hEDS. Earlier diagnosis needs to occur in order to monitor those affected with life–threatening vascular complications and provide proper therapies and treatment modalities to prevent musculoskeletal injuries. Medical schools need to improve EDS education, awareness and training. Never would I want my son, daughter or granddaughter to be caught off guard with a vascular injury out of nowhere threatening their life as I was.”- Margaret E.
“I wish my 25-year-old self had trusted my intuition more and asked more questions of the medical profession. I always knew there was an underlying physical reason for the discomfort I felt when trying to live an ordinary life.” – Jennifer A.
“I wish I would have known I had EDS. That’s it. Not just only to learn how to live, physically, in a hypermobile body, but the psychological toll of being fed an inaccurate narrative about me to me is beyond belief. I am still working through grief. It is not a linear process. I can’t tell you how many times I have been told my GI issues were psychological. I was told my dysautonomia symptoms were panic attacks, and I was fed benzos (that only further messed up my GI system and never helped). Even after a recent supraventricular tachycardia episode on public transit, a self-proclaimed EDS-aware doctor insinuated I was experiencing a panic attack. I wasn’t. These stories are endless. After I was diagnosed last year, I had hoped I would finally get appropriate care. It’s still a challenge as specialists, for the most part, only see EDS as it relates to their specialty. We need a team approach. Have grand rounds together. Let’s learn from each other.
When I’ve listened to male friends and their age-related health concerns, I started to notice none of my male counterparts ever complained about being heard or believed. I am underwhelmed by this observation. Again, these issues are systemic, and I don’t know the answer. I only know, when I waiver in courage to speak up for myself, it’s not just about me; it’s about all zebras. I find the strength I need to ask the hard questions because I don’t want anyone to have to experience what I have in the first 50 years of my life on this planet.” – Elizabeth M.
“Aging is hard enough on a body, and when you add EDS, it is more complex. Five things I would tell my younger self:
1) Do everything you can to preserve your ‘healthy’ younger body.
2) Stay active, but don’t exercise in ways that can potentially harm your body.
3) Maintain a healthy weight and avoid undue stress on your joints.
4) No ‘party tricks’ or contortions that damage joints.
5) Don’t shrug off your injuries and pain; they are not typical; look to doctors for an answer.” – Kathryn S.
“ I wish I knew just how fast EDS progresses. If I had known, I probably would not have pushed my body to the limit a lot of times! I wish I knew how much strength I really had. I would have appreciated everything I was able to do without taking it for granted! I wish I would have known that my body was gonna put me down, and disability was coming sooner than I thought. And I would have made better financial decisions so that I would better be able to take care of myself as I get older.” – Pashondra J.
“I definitely would have been less active as a kid. I didn’t know about EDS back then and was always told to live with my health issues, or you were some kind of ‘wimp.’ I think my younger self kept trying to fight through health issues and stay active because I was listening to other people. I wish now I would have listened to my body and acted accordingly as I feel my body would be in a better condition now, at my current age, to maintain with EDS.” – Jim B.
“I wish I had kept current with educational events sponsored by all the educational organizations for EDS. I would have learned about neurosurgeons for EDS and cervical spine instability two years earlier. I was eventually referred to my dedicated neurosurgeon and diagnosed with atlantoaxial (C1-C2), C5-C6 and C4-C5 instability and disc bulge pressing on my spinal cord. These ligament injuries occurred from two car accidents when I was 46 and 48 years old, respectively. I became severely disabled from the injuries. After three cervical vertebrae fusion surgeries, I am going through PT to strengthen my neck to go upright without a cervical collar. I get intense muscular headaches due to trigger points if I overdo it, but my physical therapist is excellent at manual therapy.” – Sonya G.
“I wish my 25-year-old self would have known that EDS was even a diagnosis. I wish I would have known that the advice I received at the time was not what someone with EDS needs; the advice was at times even contraindicated.” – Isabel R.
Question 5: What are the top five things that help you with your symptoms related to aging with EDS?
“1. Accepting my personal physical limitations has been a priority for me as I have aged. I spent too many years of my life trying to look like I wasn’t suffering on the outside.
- Finding just one person who is interested enough and finds me worth listening to during times of stress and physical discomfort is so important. I have that person in my life (my daughter); I keep her close and never take her for granted. I feel for those who don’t have that person in their lives.
- Listening to music with good quality noise-canceling headphones.
- Regular gentle exercise and walking my little dog when I can, and accepting the days that I can’t without beating myself up mentally on those days.
- A great consultant physician with the necessary expertise in EDS/PoTS to answer questions (unfortunately recently retired).” – Jennifer A.
“1. Having extensive medical records so that I feel I have an easier time convincing docs.
- Facebook support and medical groups. Twitter contacts with EDS specialists, research.
- Now using bracing and taping for the first time, starting about five years ago.
- Being able to not work – to finally take the time I need to manage day to day. (Self-employment for the last 20 years)
- Having folks listen.
- And I think more appropriately as a sixth question: What are the topfive things that would help? Purchase of items not covered by Medicare. Easier travel to experts as driving myself is very difficult at this point. Assistance finding appropriate specialists when one has a conservative and not highly knowledgeable PCP. Shortening the time to get to appropriate specialists. Gaining support of the healthy in my age group. Otherwise, one is completely isolated.” – Delia W
“1. Being brutally honest about the energy cost of an activity, whether it is grocery shopping or a trip to visit family.
- 2. My service dog not only helps me by performing tasks, but he connects me to the Canine Companions service dog community. He is a source of unending joy.
- Powerchair: I never have to wonder whether the walk will be too far or the stand too long.
- Morning walks on my very flat driveway. While walking in one direction is harmful to me, alternating walking backwards, then forward, then sideways is very helpful. My 11-year-old retired service dog thinks these walks are lots of fun, so we do it together. My husband says it looks like we are dancing.
- Finding a purpose that I love. Learning and using my brain is what gives me purpose and makes me feel alive. Find what makes your heart sing. – Jeannie M.
“1. Jeannie Di Bon’s Zebra Club app is my lifesaver. Her Integral Movement Method is the only type of PT that has made sense to my body and allowed me to move from pain to Grace.
- Bendy Bodies podcast, with Jennifer Milner and Dr. Linda Bluestein, has given me an invaluable resource to learn, connect and have some reference point to not feel so alone through this journey. I cannot tell you how many times painsomnia has had me by the throat in the wee hours, and knowing I can tune in and not feel so alone while the rest of the world is still sleeping, has saved me.
- The book Disjointed: Navigating the Diagnosis and Management of Hypermobile Ehlers-Danlos Syndrome and Hypermobility Spectrum Disorders edited by Diana Jovin is number three on my list. I am still studying it.
- Medical Cannabis: I cannot express how grateful I am that I let go of my misperceptions about medical marijuana and started educating myself more.” – Elizabeth M.
“1. Proper pain relief
- Dry needling (to reduce muscle spasm)
- Having activities that make me happy and aren’t too exhausting physically.
- Appropriate nutrition and keeping my weight in balance. A lot of laying down, little physical activity, and the inclination to eat away frustration… it’s a challenge.
- Progressive is progressive. Knowing about the things that are ahead and being prepared for the circumstances you will be confronted with softens the blow that will come.” – Han de V.
“Other than my pain meds, a careful diet and my walking stick, I have found ways to cope with becoming more limited in what I can do. I tend to plan my day better now than I did before. One thing that has helped me cope is my varying levels and types of advocacy work and also my creative writing. Also watching short videos, movie clips and other sources of distraction that help lift my spirits. Last thing I’ll say is that having such a long period of time of not being well, it has prepared me for the aging process since I felt like I was 60 when I was 30. There is no better teacher than one you see every day.” – Jon R.
“1. Ramps in my home for the times I’m on crutches.
- Keeping ergonomic crutches (with shock absorbers) within reach of my bed, for those times I awaken with new strains and sprains, which keep me from being able to bear weight on my legs.
- Water exercise helps keep my muscles toned but is gentle on the joints.
- Maintaining a sense of humor. It helps you to keep perspective. Like the time I read that people with EDS can touch their foot to their head. As my husband walked by, I said, ‘I just read people with EDS can touch their foot to their head. Hey, look, I can do it! Is that a common thing? Can you do it?’ He tried and concluded that he could take his shoe off and touch his SHOE to his head, but not his foot. We laughed.
- Figuring out a fun hobby I can do while lying down. In my case, I took up art for those frequent times my Dysautonomia and/or EDS causes me to be stuck in bed. That way, instead of feeling frustrated about all the things I want to be doing but physically cannot, my attitude is ‘Well, guess it’s time to have some fun creating artwork.’ Little did I know that the art I began doing for this reason in 2017 would end up being in art galleries, gift shops, a book cover, a poetry book, and, more recently, a museum exhibit. I even eventually taught myself – while lying down – how to make an art website so I could sell online. You really never know what life is going to bring, do you? – Melissa M.
“1. A hobby (painting) that I love helps to distract me from the pain.
- Meal planning for my work week, so I don’t have to cook on my workdays as the pain is unbearable by the end of the day.
- Heating pad, retractable walking stick for long walks.
- Various braces for knees, wrists, feet, elbows. I have a whole bag full; good K-tape for my feet and calves.
- Pain meds, topical pain relief, meds for breathing and heart.”- Monica H.
“The best things that help actually relate to the “trifecta” of mast cell activation syndrome (MCAS), postural orthostatic tachycardia syndrome (PoTS), along with hEDS.
(1) Lifestyle and specifically my (2) diet changes: Adhering to a very healthy plant-based diet has actually made my body function better. There is so much overlap in these conditions. Mast cell disorders affect joint health, inflammation, nerve problems, and connective tissues. The (3) things I avoid due to mast cells also help EDS: friction, exercise, stress, body temperature, certain meds, inflammatory foods, and caution with types of medical procedures or surgery. Understanding this link has been crucial to managing both conditions.
(4) Plant–based medicine (cannabis) for pain management, which I find much healthier than pharmaceuticals (although I rely on these too).
(5) Movement: the best thing my geneticist said was, “NO LAND PT, WATER ONLY!” Physical therapy might be dangerous to those with EDS, especially in the hands of non-experienced therapists. Water takes the strain off the joints while allowing for gentle movement and strengthening slowly.” – Wilder E.
For a more appealing presentation of this project,
Click HERE [Link to Presentation]
This was…
The EDS & Aging Project
If you liked this project, please share it!
Have any recommendations? Let us know!





















I find it interesting that most of the group didn’t know what EDS was when they were 25 (I certainly didn’t) and were diagnosed much later in life. Perhaps now that diagnosis in the teens or early 20s is more common, issues related to aging will be different for them after a lifetime of proper management rather than a lifetime of trying to push through it.
As a 58-year-old EDSer, thank you for this meaningful project. I hope additional projects and studies will be added because most of my well-respected EDS knowledgeable doctors still believe the concept that EDS itself is not the factor that causes the worsening of issues with age. They typically blame it on such things as arthritis. But the truth is that EDS/hypermobility has to be the cause.
When I was diagnosed over ten years ago, my geneticist told me my EDS symptoms should improve as I aged. Boy, was she wrong! My tendons are more prone to tears, my spine and larger joints are more hypermobile, which causes more pain, my fatigue is worse and sometimes becomes debilitating,, and facial pain is a constant battle. Dr. Castori et al. conducted some research on the progression of EDS/JHS around 2011-2013 and published their results, but these articles are now behind a paywall.
Understanding what happens to EDSers later in life should also help us access better pain management.
As a 42 year old newly diagnosed EDser, so much of this resonated. Also, I took many notes to hopefully ease some of the strain that comes along in Zebra aging. Thank you!
I enjoyed reading this article. And totally agree that most people have no idea what we go through each day. My mother is 83 and has EDS, hypermobile type and so do I. At 59 it is usually a struggle each day just to get out of bed. Also agree that most drs have no idea how EDS impacts ALL of our body