Lack of Clinical Understanding about Hypermobility Conditions and Treatment
By Bill Schu.
Many doctors do not understand the clinical significance of joint hypermobility. This has a major impact on accessing appropriate treatments.
 Mobility is great. Hypermobility? Less great. In the joints, hypermobility leads to musculoskeletal pain – and often times, lots of it. A recent review in the Journal of Pain Research outlined several of the challenges in treating generalized joint hypermobility (GJH) and found many difficult questions and few easy answers.
Mobility is great. Hypermobility? Less great. In the joints, hypermobility leads to musculoskeletal pain – and often times, lots of it. A recent review in the Journal of Pain Research outlined several of the challenges in treating generalized joint hypermobility (GJH) and found many difficult questions and few easy answers.
Hypermobility syndrome (HMS) is often the key suspect in cases of chronic pain where no other conditions appear to be causing it. Researchers and clinicians have struggled for decades with the highly diverse clinical presentation of HMS, and many are unaware of it altogether.
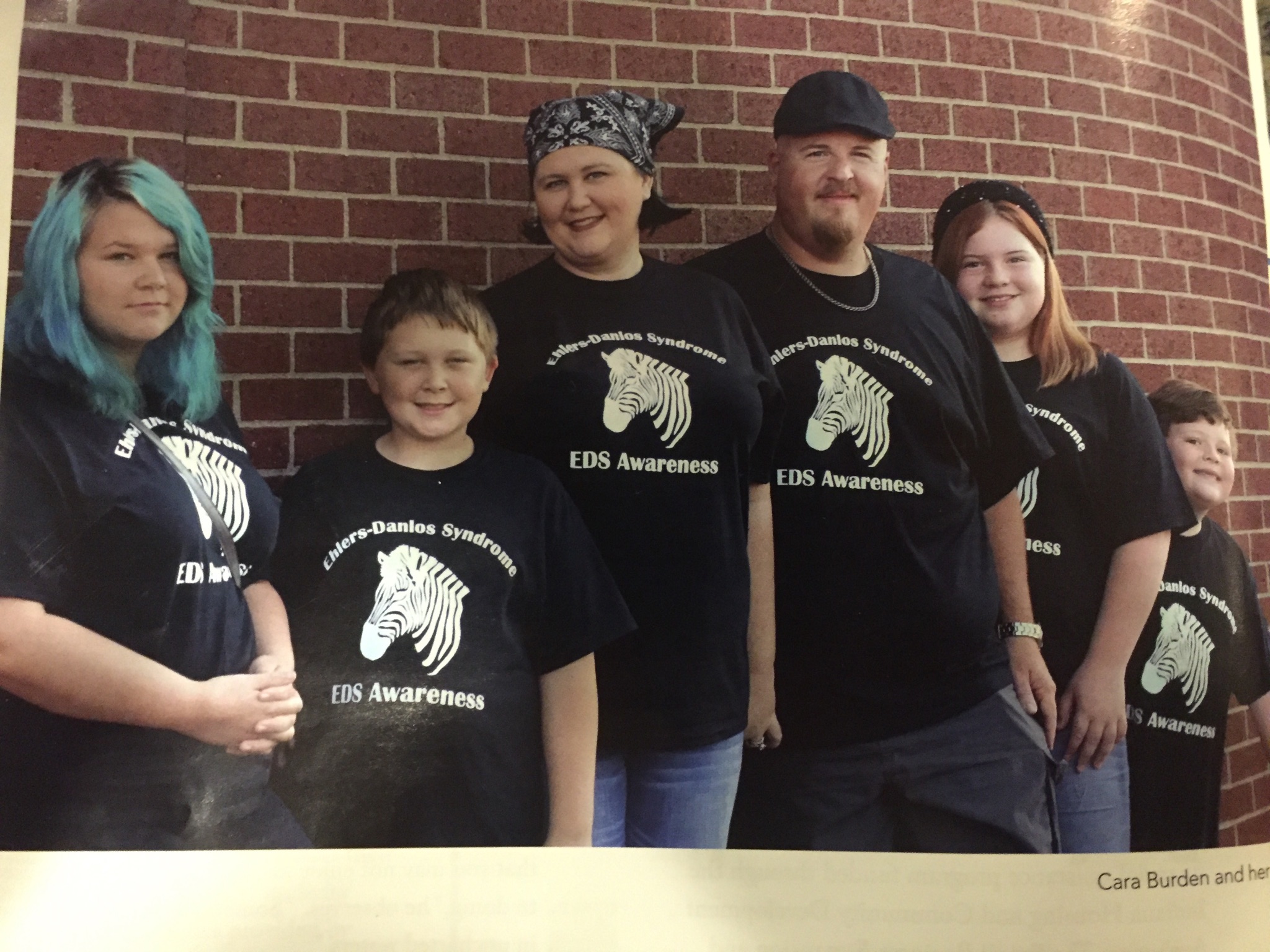
“Patients tend to search for years within the medical system before a diagnosis is established,” noted the review authors – adding that it remains surprising that HMS is often overlooked although it may affect as many as 57% of the general population and certainly a significant number of patients suffering from chronic pain. GJH is frequently present in hereditary diseases of the connective tissue, such as the Marfan syndrome, osteogenesis imperfecta, and the Ehlers–Danlos syndrome hypermobility type (EDS-HT).
The review succinctly presented the condition in terms of three key challenges, and then suggested some potential solutions for those challenges.
Challenge 1: Because of its clinical heterogeneity, HMS/EDS-HT is underdiagnosed and poorly understood.
GJH is highly prevalent among athletes, dancers, martial artists, and gymnasts, as well as among other professionals in performing arts Therefore, it is often not seen by either patients or practitioners as a clinical sign associated with disease. Although these groups are at higher risk of developing musculoskeletal pain, they are still able to demonstrate high levels of physical performance and motor control. Yet, earlier studies show that GJH has a profound effect on many, in terms of musculoskeletal pain, fatigue, deconditioning, and psychological distress.
Possible solution: Revising diagnostic criteria and establishing international consensus. Current diagnostic criteria have been in place for decades, but they are controversial, and thus, clinical consensus has been a problem.
Challenge 2: Although many theories have been promoted regarding why individuals with GJH develop chronic pain, no single pathophysiological model has been identified.
Generalized joint instability may cause the occurrence of microtraumas on joint surfaces, leading to adaptation and compensation of movement patterns, consequently causing overload in other areas of the movement apparatus. The exact mechanisms of disease are not yet well-understood.
Possible solution: By developing and using subgroup classifications, the variability in diagnosis and treatment could be reduced. This would be similar to recent approaches in the diagnosis and treatment of back pain, which have been very effective. For hypermobility conditions, however, this will require a great deal of future research into exactly what those subclassifications should be.
Challenge 3: Within the HMS/EDS-HT phenotype, there is a high prevalence of psychosocial factors.
“As in other chronic pain syndromes, it seems that apart from biomedical factors, psychosocial factors also contribute to a person’s eventual level of disability,” the review authors noted. “It could be that pain-related fear will also have an accumulating disabling effect in hypermobile persons with pain.”
Possible solution: Although no individual step will solve for this challenge, the review authors advised that development of a clinical core set would enable creation of disease-specific reference values. This would enable clinicians and researchers to compare results around the world, which would ultimately lead to improvement in patient care.
“The specific problems associated with the GJH-related syndromes, as compared to other chronic pain syndromes, are still challenging for most physicians and other health personnel due to many issues surrounding etiology, disease classification, diagnostics, and treatment,” the authors concluded. “Lessons learned from other fields of chronic pain management should be considered.”
More education and awareness is needed for the medical community to develop a better understanding of hypermobility conditions such as Ehlers-Danlos Syndrome.
Click here for the original source of this article
We appreciate your Facebook shares, likes and comments