This month we are going to dive into cerebral venous outflow disorders, and why they should be on your radar. We’ll also take a look at a new small study showing how cerebral venous outflow disorders may present differently in those with connective tissue disorders (like Ehlers-Danlos syndromes). Lastly, we’ll discuss diagnostic and treatment challenges, support, and where you can learn more.
But First… a Small Lesson on the Brain’s Plumbing System
In order for our brains to remain happy and healthy, various fluids need to flow freely in and out of the brain in an unobstructed fashion. Our arteries supply our brains with fresh oxygenated blood, while our veins drain deoxygenated blood out. Cerebrospinal Fluid (CSF), a clear liquid surrounding the brain and spinal cord, keeps our brain and spine cozy and protected, while also removing waste. When something obstructs blood or CSF from leaving the brain properly, intracranial pressure can elevate causing a range of complications and symptoms.
What are Cerebral Venous Outflow Disorders?
Most doctors understand the serious consequences of arteries in our head or neck becoming blocked, stenosed, or ruptured, as these can lead to stroke. In contrast, impaired venous drainage has historically been under-researched and poorly understood. In the last few years, however, there has been a growing interest in what experts are referring to as cerebral venous outflow disorders. While not yet a formalized medical term, top researchers and experts in the field, including groups such as the Society of Neurointerventional Surgery, have begun to use this name to describe a spectrum of conditions related to issues with how fluid drains from the brain. Much like how a clogged drain causes water to rise or overflow, narrowing or blood pooling of the veins in the head or neck can cause fluid pressure to build up around the brain. Idiopathic Intracranial Hypertension (IIH) is considered the most well-known of these conditions.
Symptoms of Cerebral Venous Outflow Disorders
Individuals with conditions associated with cerebral venous outflow disorders report experiencing a wide variety of symptoms such as:
-
- pressure headaches (that often worsen when lying flat)
- dizziness
- ringing tinnitus and pulsatile tinnitus (a rare vascular form of tinnitus)
- neck pain
- tenderness at the base of skull
- vision disturbances
- brain fog
- cognitive dysfunction
- sleep disorders
- choking sensations
- The quality-of-life impact of these symptoms can vary widely from person to person. For some they can be debilitating. With severe, untreated intracranial hypertension, blindness can even occur.
Associated Conditions
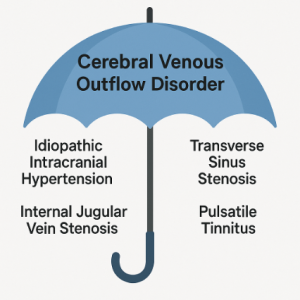
As mentioned above, cerebral venous outflow disorders are a relatively new umbrella term for conditions that impair how fluids drain from the brain.
Conditions under the “cerebral venous outflow disorder” umbrella are:
Can You Have More Than One Associated Condition?
Yes! Patients can have more than one of these conditions, often with one causing the other. For example, if muscles or other bony structures in the neck compress the internal jugular vein, blood cannot smoothly exit the brain (for example, internal jugular vein stenosis). This, in turn, could lead to IIH, or cause vessels in the head to ‘balloon’ upstream, which could lead to pulsatile tinnitus.
Why This Matters for EDS Patients
Ehlers-Danlos syndromes (EDS) are a collection of 13 heritable connective tissue disorders (CTDs). In recent years, experts have observed that cerebral venous outflow disorders and CTDs frequently go hand-in-hand, but more research is needed to understand why.
Furthermore, a recent small study revealed that IIH (a condition under the cerebral venous outflow disorders umbrella) may have a distinct clinical presentation when it shows up in individuals with CTDs. Typically, IIH occurs in “obese women of child-bearing age, with diverse racial backgrounds”. In most cases, losing weight can spontaneously reverse it. However, a 2024 retrospective study from Wake Forest School of Medicine found that patients presenting at their clinic with both suspected IIH or another cerebral venous outflow disorder, and a CTD, did not fit the classic IIH patient profile. While these patients were still predominantly women (87%), most were not obese, and almost all were white (90%). Perhaps even more importantly, diagnosing IIH typically requires patients to have high opening lumbar pressures (≥ 250 mmCSF) and papilledema (swelling of the optic nerves in the eyes). These patients, instead, had opening lumbar pressures less than 250 mmCSF and a significantly lower occurrence of papilledema (20%). Despite this, these patients with CTDs still had the same classic symptoms typically associated with IIH, such as dizziness, headaches, tinnitus, and cognitive dysfunction. However, they reported more severe headaches and a worse quality of life than those without CTDs. The results of this study suggest that patients with CTDs may be more sensitive to venous congestion in the brain or changes in intracranial pressure. However, further research is needed to confirm this.
Diagnostic Challenges
CTDs (in particular hypermobile EDS (hEDS) or hypermobility spectrum disorders (HSD)) can have many overlapping symptoms with cerebral venous outflow disorders. There are also many health conditions that often co-occur with hEDS or HSD, such as postural orthostatic tachycardia syndrome (POTS) or mast cell activation syndrome (MCAS), that can have similar symptoms to cerebral venous outflow disorders. This makes it difficult to identify whether symptoms are stemming from one, or even several, conditions. This can delay diagnosis and treatment considerably.
Furthermore, as highlighted by the small study discussed above, those with CTDs may not meet typical diagnostic criteria for conditions like IIH. Thus, these individuals could face obstacles in receiving further medical testing, despite their severe symptoms.
Even with these diagnostic challenges, awareness is growing, and finding a specialist who understands these conditions can help patients get the support they need.
Treatment
As cerebral venous outflow disorders encompass a variety of conditions, there is no one-size-fits-all treatment. For many patients, more conservative treatment options (such as medication or physical therapy) may offer relief and should always be considered as the first line of care. In patients who experience debilitating symptoms, surgical intervention could offer some benefit. However, experts warn that criteria concerning who should receive such surgical intervention, and at what stage, is currently poorly defined, and evidence supporting surgery is still very limited. Allergies to adhesive tape, sutures, or certain medications are also common in the EDS community, adding a further layer of caution.
(Chronic Pain Partners has written an article about surgery prep here.)
What if You Suspect This Condition?
If these symptoms sound familiar to you, advocate for yourself and share this article with your clinician. While the terminology and research are still evolving, building awareness in your community about conditions that affect brain drainage, especially for those with CTDs, can help speed progress toward a brighter future with better diagnostic testing and treatments!
Support
Dealing with symptoms due to cerebral venous outflow disorders can feel tough and isolating. You don’t have to navigate this alone! As international awareness has grown amongst experts and patients, so too have support groups increased in number around the world. While there are not any groups yet for cerebral venous outflow disorders specifically, there are some wonderful social media support groups for many of the associated conditions. For example, the Jugular Venous Outflow Disorders (Cerebral Venous Congestion) Facebook Group.
Where Can You Learn More?
Thankfully, there are some great resources to help you learn more. In 2022, the Society of Neurointerventional Surgery (SNIS) formed the Cerebral Venous and CSF Disorders Committee. They now host yearly summits where many of the top experts from around the world present new findings.
2026 SNIS Cerebral Venous and CSF Disorders Summit:
Other Great Webinars From 2022 and 2025 Featuring Top Experts:
The Takeaway
- The term cerebral venous outflow disorders refers to a group of conditions that impair fluid drainage of the brain, with IIH being the most well-known.
- Brain drainage issues can cause a host of symptoms such as pressure headaches (that often worsen when lying flat), dizziness, pulsatile tinnitus (a rare vascular form of tinnitus), neck pain, tenderness at the base of skull, vision disturbances, ‘brain fog’, and cognitive dysfunction
- Experts have started to observe a connection between connective tissue disorders (CTDs) (like hypermobile EDS) and cerebral venous outflow disorders, but research is needed to understand why.
- Idiopathic intracranial hypertension (a condition under the cerebral venous outflow disorder umbrella) may look different when it presents in individuals with CTDs than individuals without, creating diagnostic challenges.
Jacqueline Teti, author
patient with HSD and cerebral venous outflow disorders
September 2025


