![]()
Previous editions of Research Round-up can be found at the following links:
Edition 5 (Pediatrics) Edition 4 (Neurodivergence) Edition 3 Edition 2 Edition 1
Howdy, partners! This Research Round-up has roped in a whole herd of topics for you. We hope you enjoy the read, learn a thing or two, and feel ready for a showdown!
Remember, knowledge is yer firepower, and ya need all the firepower ya can get. Now git along and read!
CARDIOVASCULAR/AUTONOMIC NERVOUS SYSTEM
Hypermobile Ehlers-Danlos Syndrome: Cerebrovascular, Autonomic and Neuropathic Features
Published in the American Journal of Medicine Open | July 18, 2025 | Link to full text
Research by Peter Novak, MD, PhD, David M. Systrom, MD, Sadie P. Marciano, PA-C, Alexandra Witte, PA-C, Arabella Warren, MD, PhD, Donna Felsenstein, MD, Matthew P. Giannetti, MD, Matthew J. Hamilton, MD, Jennifer Nicoloro-Santa Barbara, PhD, Mariana Castells, MD, Khosro Farhad, MD, David M. Pilgrim, MD, William J. Mullally, MD, Mark C. Fishman, MD, Jeff M. Milunsky, MD, Aubrey Milunsky, MD, and Joel Krier, MD
Summary: This research article investigates the cerebrovascular, autonomic, and neuropathic features of hypermobile Ehlers-Danlos Syndrome (hEDS). Analyzing 270 hEDS patients against patients without hEDS, the study found significant evidence of abnormal or reduced control over blood flow to the brain, which correlates with symptoms like dizziness. Furthermore, a high prevalence of small fiber neuropathy (damage to the small nerve fibers in the body) and widespread, albeit mild, autonomic failure affecting multiple bodily systems (cardiovagal [34.4% of hEDS patients], adrenergic [69.3%], and sudomotor [57.1%]) was observed in hEDS patients, highlighting the complex, multisystem nature of the syndrome and identifying potential new targets for treatment.
Related: Learn more about cerebral venous outflow disorders and their relationship with EDS.
The utility of the implantable loop recorder in patients with Ehlers-Danlos syndrome and hypermobility spectrum disorder
Published in the Journal of Osteopathic Medicine | June 19, 2025 | Link to full text
Research by Ermin Tale, DO, Grace Robinson, BS, Justin Edward, BS, Riya Kaushal, BA, Bernadette Riley, DO, MS, and Todd J. Cohen, MD
Summary: This study investigates the utility of implantable loop recorders (ILRs) in diagnosing and managing arrhythmias in patients with Ehlers-Danlos Syndrome (EDS) and hypermobility spectrum disorders (HSD). These patients often experience cardiac symptoms like palpitations and presyncope, sometimes attributed to postural orthostatic tachycardia syndrome (POTS), but the cause can be unclear. Researchers conducted a retrospective analysis of 116 hypermobile patients, finding that ILRs were effective in identifying symptomatic arrhythmias such as sinus tachycardia, premature ventricular complexes, and supraventricular tachycardia. Furthermore, ILR monitoring proved valuable in solidifying POTS diagnoses and guiding treatment efficacy, leading to crucial interventions like ablations and device implantations in some cases. The study concludes that ILRs are a beneficial tool for long-term cardiac monitoring in this specific patient population, though it recommends further research with larger cohorts.
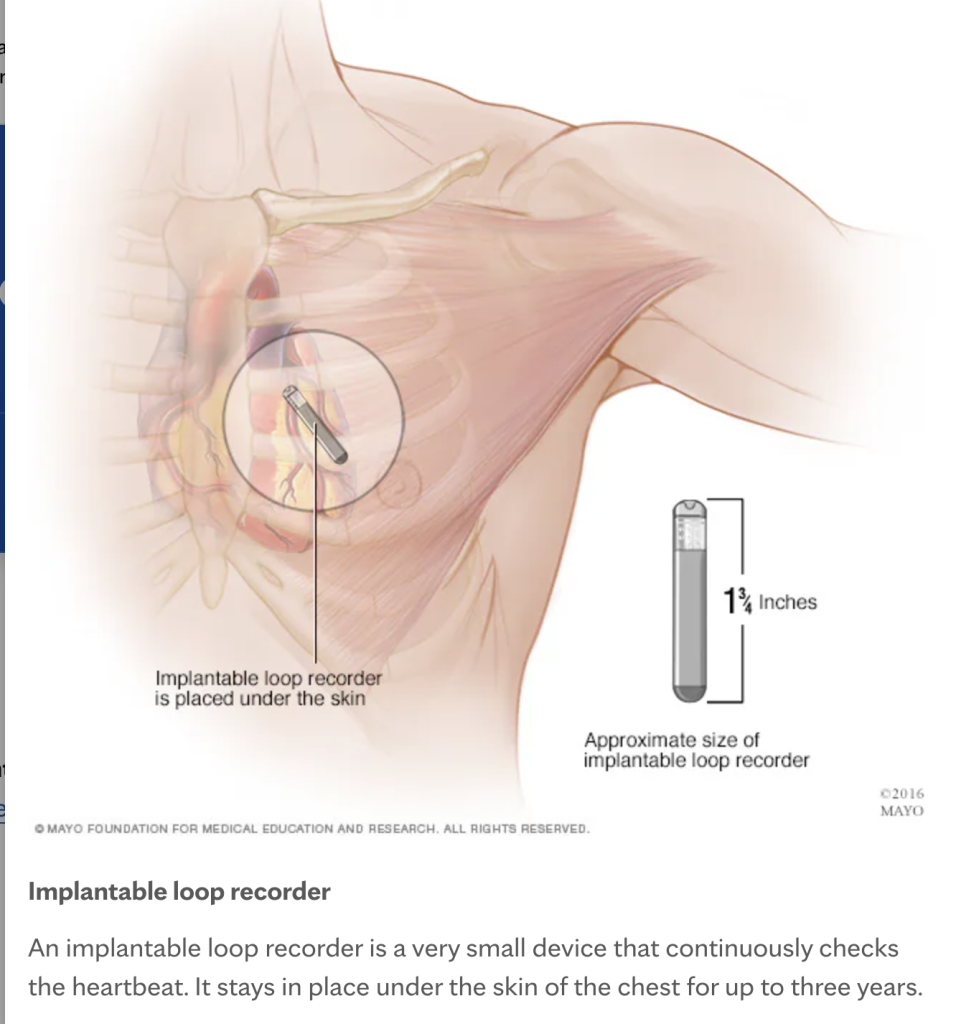
A loop recorder is implanted under the skin near the patient’s heart.
DIAGNOSIS
The Contradictions in the Criteria for Diagnosing Hypermobile Ehlers–Danlos Syndrome as Reflecting Some of the Philosophical Debates about the Threshold between the Normal and the Pathological
Published in The Journal of Medicine and Philosophy | April 16, 2025 | Link to full text
Research by Mar Rosàs Tosas
Summary: This article delves into the contradictions within the diagnostic criteria for hEDS, arguing that these inconsistencies mirror broader philosophical debates about defining disease. There are three major inconsistencies the author identifies. First, the author discusses whether a disease is a naturally occurring, measurable state (a theory called “naturalism”) or if it is a social construct, made up by humans and intertwined with human values and morals (a theory called “normativism”). Second, the author highlights how the changing and restrictive diagnostic criteria for hEDS lead to patients being “let in and out” of the diagnosis, causing significant skepticism from others. It also causes the patient mental anguish because others do not consistently consider them “sick” or “sick enough,” which limits their access to resources intended for people in those categories. Third is the problem of “line-drawing”—establishing a sometimes-arbitrary boundary between health and illness, as well as determining what qualifies as a symptom of hEDS and what does not. For example, a person can have all but one symptom of hEDS, and they will not get a diagnosis. This contrasts with HSD, which exists on a spectrum and can accommodate people with a variety of symptoms and severity. Ultimately, the piece advocates for healthcare professionals to acknowledge that the diagnostic criteria is a guide, emphasizing that medicine can and does function effectively even without definitive labels, thereby reducing the harm experienced by patients.
Related: A new study by Dr. Pradeep Chopra reveals how misdiagnosis can harm patients with EDS. Turns out, it’s not all in our heads.
GASTROINTESTINAL
Association Between Ehlers-Danlos Syndrome and Celiac Disease
Published in Gastro Hep Advances | June 5, 2025 | Link to full text
Research by Nana Ama Adjei-Frimpong, Francesco Delacqua, and Reid Oldenburg
Summary: This research investigates a notable connection between celiac disease (CD), an autoimmune condition triggered by gluten, and EDS. Utilizing a large-scale U.S. database called “All of Us,” the study found a significantly increased likelihood of EDS diagnoses in individuals with CD, an association that remained robust even after accounting for other autoimmune diseases. The authors suspect that connective tissue dysfunction inherent in EDS may affect the walls of the intestines, making that barrier weaker. This could potentially predispose individuals to autoimmune responses like those seen in CD. This study provides new insights, differing from previous smaller European studies, and emphasizes the need for clinicians to consider this link and for further research into shared genetic and immunological pathways.
Related: An article summarized later in this Round-up discusses what role fascia plays in hEDS and HSD bodies, including involvement in GI issues.
HYPERMOBILITY SPECTRUM DISORDER
Localized and historical hypermobile spectrum disorders share self-reported symptoms and comorbidities with hEDS and HSD
Published in Frontiers in Medicine | August 13, 2025 | Link to full text
Research by DeLisa Fairweather, Katelyn A. Bruno, Ashley A. Darakjian, Frances C. Wilson, Jessica J. Fliess, Emma F. Murphy, S. Christian Kocsis, Max W. Strandes, Gabriel J. Weigel, Alayna M. Puls, Cameron J. Hartmoyer, Charwan Hamilton, Emily R. Whelan, Jessica M. Gehin, Stacey M. Menton, Hanna Sledge, David O. Hodge, Shilpa Gajarawala, Bala Munipalli, Chrisandra L. Shufelt, Paldeep S. Atwal, and Dacre R. T. Knight.
Summary: This study investigates whether localized and historical hypermobile spectrum disorders (L-HSD/H-HSD), which involve hypermobility in specific areas of the body or past contexts, share symptoms and comorbidities with hEDS and HSD. The researchers analyzed self-reported data from a large patient cohort who filled out the 300-question REDCap Intake questionnaire at Mayo Clinic Florida EDS Clinic, which is given before first appointments. They looked at 100 symptoms and comorbidities. The researchers found that L-HSD/H-HSD patients exhibit a similar and, in some cases, even greater burden of symptoms and comorbidities compared to those with hEDS or HSD. This suggests that the current diagnostic criteria for hEDS and HSD may need revision to incorporate L-HSD/H-HSD more fully within the HSD diagnosis, ensuring these patients receive appropriate care and are included in future research efforts. The paper also highlights an intriguing observation that hEDS patients, diagnosed by a physician expert using the 2017 hEDS criteria often report fewer systemic symptoms than those with HSD and L-HSD/H-HSD. The authors speculate that this may be due to the 2017 hEDS diagnostic criteria inherently selecting for patients who have more specific structural symptoms than body-wide symptoms, leaving the latter group with a diagnosis of some form of HSD. They also speculate that L-HSD and H-HSD are less likely to visit a specialty clinic unless they present severe symptoms, leaving those with more minor burdens out of the study.
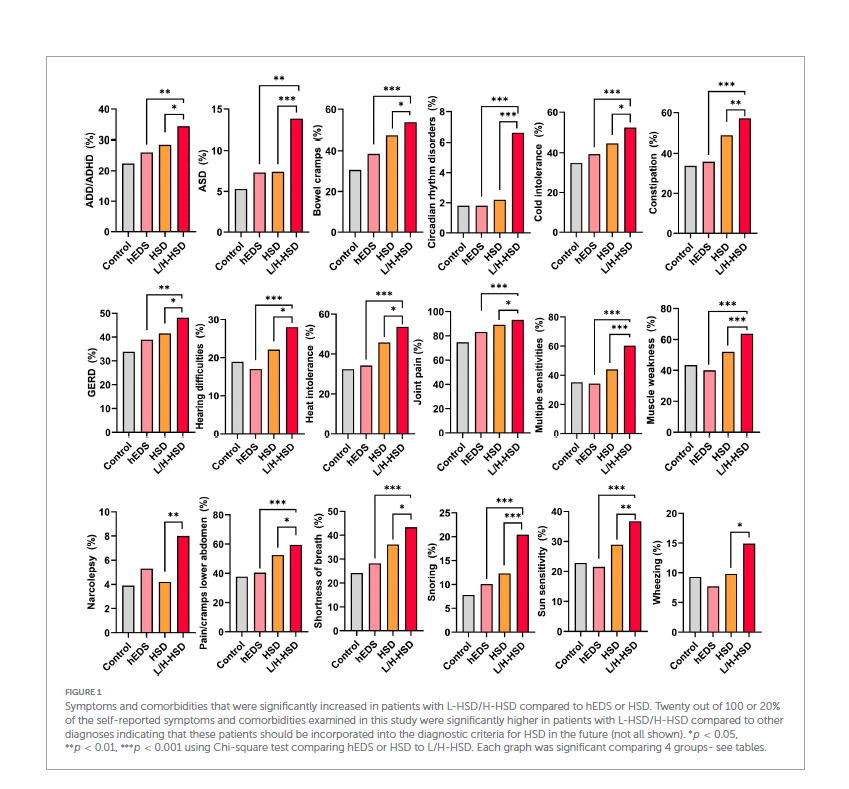
The graphs show 18 of the 20 symptoms that were significantly increased in people with L/H-HSD compared to those with hEDS/HSD. The names of the conditions are listed to the left of the graphs.
MISCELLANEOUS
Health care supply in patients with Ehlers-Danlos syndromes and generalized hypermobility spectrum disorder: a German perspective
Published in the Orphanet Journal of Rare Diseases | August 16, 2025 |Link to full text
Research by Jonas Rauterberg, Marie Hock, Nikolaus Kernich, Arim Shukri, Henning Klapproth, Vanessa Löw, Michaela Henning, and Iliana Tantcheva-Poór
Summary: This research article investigates the diagnostic journey and the individual, community, and societal impacts of EDS and HSD on patients in Germany, a region previously lacking specialized EDS services. Through a survey of patients from a newly established EDS outpatient service at the University Hospital of Cologne, the study reveals a significantly long “diagnostic journey”—an average of 22 years. (The average time to diagnosis in the United States is around 14 years.) The study also found high rates of comorbidities: 78.6% of patients reported having at least one other diagnosis. The most common additional diagnoses were asthma (21.4%), depression (21.4%), irritable bowel syndrome (14.3%), and POTS (13.3%). Pain, orthopedic problems, gastrointestinal complaints, and fatigue were reported as the top four symptoms affecting daily life.
Substantial utilization of healthcare services was also reflected, including:
- The average number of medical specialties an EDS patient needed for diagnosis and management: 15 specialists
- Number of surgical interventions: a mean of five per patient
- Use of physical therapy: 94.9% of patients had at least one appointment.
- Use of psychotherapy: 68.7% received psychotherapy in their lifetime compared to a rate of 24.5% self-reported by adult Germans with a mental disorder.
- Use of splints and orthoses: 66.7%
- Use of pharmacotherapy: opioids were reported as being used by 15.5% of the respondents and non-opioids by 83.5%.
The authors conclude that these findings emphasize the need to provide better coordinated, multidisciplinary care for EDS/HSD patients in Germany, along with further research and improved political structures to address the complexities of these conditions.
Fascial Pathophysiology in Hypermobility Spectrum Disorders and Hypermobile Ehlers–Danlos Syndrome: A Review of Emerging Evidenc
Published in the International Journal of Molecular Sciences | June 11, 2025 | Link to full text
Research by Tina J. Wang, Antonio Stecco, Alan J. Hakim, and Robert Schleip
Summary: This review explores the pathophysiology of fascial tissues in HSD and hypermobile Ehlers–Danlos Syndrome (hEDS). Fascia was once considered merely a passive support structure. Research is now finding that it is a changeable type of multi-layered connective tissue with nerves, blood vessels, and its own extracellular matrix. Fascia is involved in the following bodily functions:
- Transmitting mechanical force (like the impact of a fall) throughout the body
- Sensing and responding to mechanical stimuli, especially stimuli that stretch (like the jerk of the leg when a knee is hit with a reflex hammer) or shear (like food that exerts pressure on the lining of the intestines)
- Proprioception—the understanding of where one’s body is in space
- Pain modulation
- Intercellular and systemic communication
- Inflammation and fibrosis
- Fluid balance
The nerve fibers in fascia are made up of about 40% autonomic nerves with high densities found around blood vessels. These nerves help with blood vessels expanding and contracting. This paper suggests that fascia could play a pivotal role in joint instability, chronic pain, and autonomic dysfunction. Therefore, if fascia is not built or working correctly, it could cause abnormalities in the thickness of the fascia, how the fascia glides against other surfaces, how tendons stretch, and tissue stiffness. Ultimately, this review aims to bridge the gap between what is happening at the molecular level and what symptoms and signs are seen in the human body, calling for further multidisciplinary research to improve diagnosis and develop targeted therapies.
NEUROLOGY/PSYCHOLOGY
Neuropsychological Function and the Relationship Between Subjective Cognition, Objective Cognition, and Symptoms in Hypermobile Ehlers–Danlos Syndrome
Published in Brain and Behavior | May 15, 2025 | Link to full text
Research by Amber Sousa, Min-Kyung Jung, Arline Allera, and Bernadette Riley
Summary: This research investigates the brain’s control over cognitive abilities, emotional regulation, and behavior in individuals with hEDS. The study compared hEDS patients to patients without hEDS on a comprehensive series of tests. It found no significant differences in objective cognition measures, which include attention, executive function, memory, and language. The hEDS group did demonstrate lower scores for delayed verbal memory recall—the type of recall used to remember a word, story, or number after a short period of time. The research also explored subjective cognitive complaints (how bad the individual thinks their memory is working) in a larger hEDS group. They found moderate correlations between the subjective cognitive complaints and hEDS patients performing worse regarding working memory and visuospatial planning (like copying a complex figure) and construction tasks. Essentially, in these two areas, if a person with hEDS thinks they are bad at a particular skill, they will do the task more poorly—but not in any of the other areas tested. Additionally, worse subjective cognitive complaints strongly correlated with more difficulty in social situations and moderately correlated with anxiety, pain, fatigue, and depression. The authors conclude that cognitive difficulties in hEDS are likely fluctuating and correspond with other symptoms, emphasizing the need to validate subjective cognitive concerns and consider comprehensive treatment approaches.
Ignored, Dismissed, and Minimized: Understanding the Harmful Consequences of Invalidation in Health Care—A Systematic Meta-Synthesis of Qualitative Research
Published in Psychological Bulletin | 2025 | Link to abstract (full text not available)
Research by Allyson C. Bontempo, John M. Bontempo, and Paul R. Duberstein
Summary: This systematic review explores the detrimental impact of symptom invalidation by clinicians on patients suffering from contested, ambiguous, unpredictable, and difficult-to-diagnose illnesses, such as EDS and HSD (20.4% of the study’s patients), long COVID (38.8%), myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) (21%), endometriosis (13.3%), and others. It highlights that such invalidation, stemming from clinical uncertainty, communication failures, and sometimes gender bias, can lead to a range of severe negative psychological and health care consequences. Shortage of primary care physicians, finances, short visit times, and intolerance of diagnostic uncertainty can cause providers to communicate in ways that can invalidate patients’ concerns. The outcomes include painful emotional states like shame and suicidality, distress surrounding medical visits, avoidance of necessary health services, and significant diagnostic delays, ultimately making patient suffering worse and hindering effective care. The study advocates for improved clinician training and healthcare quality evaluation to counteract these harmful practices.
Related: To learn more about the effects of dismissive doctors and uncertain clinical encounters, check out our Clinician-Associated Trauma series.
NEUROLOGY/SPINE
Head Posture and Upper Spine Morphological Deviations in Patients with Hypermobile Ehlers–Danlos Syndrome
Published in Orthodontics & Craniofacial Research | February 12, 2025 | Link to full text
Research by Ashkan Jasemi, Eva Fejerskov Lauridsen, and Liselotte Sonnesen
Summary: This research article investigates the relationship between hEDS and morphological deviations of the upper spine, along with head posture. The study compared hEDS patients to healthy controls, finding that hEDS patients significantly more often exhibited abnormalities in their upper cervical spine structure, particularly posterior arch deficiencies and partial clefts. The rate of fusion anomalies was not significantly different between patients with hEDS and without hEDS. There was also a notable tendency for hEDS patients to have a more extended head posture, based on the measurement of several angles as described in the paper. Differences in craniofacial morphology included less maxillary prognathism and mandibular prognathism and a larger cranial base angle. These findings suggest that issues with upper spine morphology and head positioning are part of the clinical presentation of hEDS, potentially aiding in earlier diagnosis and more tailored treatment approaches for individuals with this complex connective tissue disorder.
Radiographic Indicators of Craniocervical Instability Analyzing Variance of Normative Supine and Upright Imaging in a Healthy Population
Published in Clinical Spine Surgery | September 23, 2024 | Link to abstract (no full text available)
Research by Alan J. Gordillo, BS, Matt Magro, BS, Derrick Obiri-Yeboah, MD, Arpan A. Patel, MD, Vorster Sarel, MD, and Alexander Spiessberger, MD
Summary: This study aimed to establish baseline ranges and variability for seven radiographic measurements of the cervical spine in healthy individuals, which can serve as potential diagnostic tools for craniocervical instability (CCI). Recognizing the researchers analyzed various imaging modalities—supine CT and flexion, extension, and neutral x-rays—from 72 non-EDS patients to address the diagnostic challenges of CCI, particularly in conditions like EDS. The findings revealed that all measurements, except the basion-axial interval and atlanto-dental interval, showed significant differences between flexion and extension x-rays. Notably, the clivo-axial angle (CXA), hard palate to C1 vertebra (HPC1), and hard palate to C2 vertebra (HPC2) were the most consistent, suggesting their potential as reliable and precise markers for diagnosing CCI.
Coming soon: Want more details about these studies and the measurements they found? We will share more details in an upcoming article.
ORTHOPEDIC
Double-Allograft Shoulder Stabilization for Multidirectional Instability Is Associated With Improved Function and Survivability After 2 Years
Published in Arthroscopy, Sports Medicine, and Rehabilitation | May 14, 2025 | Link to full text
Research by Felix H. Savoie III, M.D., Matthew W. Cole, M.D., Lacee K. Collins, B.S., J. Heath Wilder, M.D., Bailey J. Ross, M.D., Michael J. O’Brien, M.D., and William F. Sherman, M.D., M.B.A.
Summary: This article introduces a new double-allograft surgical technique from Tulane Univeristy. This treatment is intended to stabilize the shoulders of patients who suffer from severe multidirectional instability (MDI) and hyperlaxity, especially when other treatments, such as previous surgeries and physical therapy, have not been successful. This technique addresses the strong sacs of connective tissue surrounding the shoulder, called capsules. First, the surgeon performs an inferior capsule plication (a folding and suturing surgical technique performed on weakened or stretched structures in the body) and a labral repair. Then the posterior capsule is stabilized. Also noteworthy, the authors created a modified Beighton score to more accurately identify patients who would benefit most from this specific procedure. Through a retrospective review, the study demonstrates that this technique leads to significantly improved patient-reported outcomes in terms of function and pain, even in challenging cases involving conditions like EDS. They report a positive rate of increased stability after two years. The research concludes that this double-allograft reconstruction offers a safe and effective solution for individuals with significant ligament laxity.
Outcomes of Total Joint Arthroplasty in Patients Who Have Ehlers-Danlos Syndrome: A Systematic Review and Meta-Analysis
Published in The Journal of Arthroplasty | January 20, 2025 | Link to abstract (no full text available)
Tejas Subramanian, BE, Robert N. Uzzo, MBA , John Lama, MS, Michael Mazzucco, BS, Simon Ortiz, BS, and Elizabeth B. Gausden
Summary: This systematic review and meta-analysis investigates the outcomes of total joint arthroplasty (TJA), also known as joint replacement surgery. The specifically look at total hip (THA) and total knee (TKA) arthroplasty in patients with EDS. The study compiles and analyzes existing research to compare complication rates in EDS patients undergoing TJA against those without the syndrome. Key findings indicate that EDS patients face a significantly increased risk of implant-related complications, such as surgeries to redo the joint replacement, instability/dislocation, and non-infected loosening following THA. After a TKA, instability, fractures in the replacement parts, and wound complications are more common in EDS patients. Despite these elevated risks, the research highlights that patient-reported outcomes generally improve for EDS patients after TJA, suggesting that while complications are more frequent, the surgery still offers a better quality of life.
PAIN
Pain intensity in anatomical regions in relation to psychological factors in hypermobile Ehlers–Danlos syndrome
Published in the Scandinavian Journal of Pain | April 6, 2025 | Link to full textResearch by Tage Orenius, Karin von Smitten-Stubb, Hannu Kautiainen, Liisa Montin, Antonio Bulbena, and Karl-August Lindgren
Summary: This study investigates the complex interrelationship between pain intensity, pain location, and psychological distress in individuals with hEDS. The research highlights that hEDS patients experience widespread and intense pain across multiple anatomical regions. Crucially, the findings reveal a significant connection between overall pain intensity and both depressive symptoms and pain anxiety. The strength of this association varies depending on the specific body area. Notably, pain in the abdomen and lower extremities showed the strongest links to depressive symptoms, while upper extremity pain did not correlate with either depressive symptoms or pain anxiety. This study emphasizes the need for healthcare professionals to consider these psychological factors alongside physical pain when developing multidisciplinary treatment programs for hEDS patients.
UK Medical Cannabis Registry: An Analysis of Outcomes of Medical Cannabis Therapy for Hypermobility-Associated Chronic Pain
Published in ACR Open Rheumatology | March 13, 2025 | Link to full text
Research by Mary Dickinson, Simon Erridge, John Warner-Levy, Evonne Clarke, Katy McLachlan, Ross Coomber, Wendy Holden, James J. Rucker, Michael W. Platt, and Mikael H. Sodergren
Summary: This study from the UK Medical Cannabis Registry investigated the effectiveness of cannabis-based medicinal products (CBMPs), including oils, dried flowers, and a combination of both, for chronic pain associated with HSD and hEDS. The median doses studied were 25.00 mg/24 hr for cannabidiol (CBD) products and 110 mg/24 hr for tetrahydrocannabinol (THC) products. Through self-reporting, direct questioning, and documentation by clinicians, the researchers observed improvements in pain severity, overall quality of life, sleep quality, and anxiety levels among 161 patients treated with CBMPs over an 18-month period. While most patients tolerated the treatment well, about a third (50 patients) reported one or more adverse events (AEs). The AEs consisted primarily of moderate side effects like headaches, fatigue, lethargy, nausea, dry mouth, and insomnia. There were no life-threatening AEs, though 99 severe AEs were reported. The findings suggest a potential benefit of CBMPs for this patient population, though the authors emphasize the need for randomized controlled trials to confirm these associations and establish causation. (Reminder: cannabis and related products are not legal everywhere. Check with your doctor and local laws before ingesting any new drugs or supplements.)
AI was used to assist in the summary of the articles.
Kate Schultz
November 2025


