Dr. Pradeep Chopra: response
to the paper on psychological
and psychiatric aspects of the
Ehlers–Danlos syndromes
EDS expert and pain specialist Dr. Pradeep Chopra contacted Chronic Pain
Partners to speak about a recently published review on the psychological
and psychiatric aspects of the Ehlers-Danlos syndromes and Hypermobility
Spectrum Disorders. Dr. Chopra has been treating complex pain patients
focusing on people with the Ehlers-Danlos syndromes for decades, and is a
passionate advocate for patients around the world.
The following is his critical review of the paper “Updates of the
psychological and psychiatric aspects of the Ehlers-Danlos Syndromes and
hypermobility spectrum disorders” by Andrea Bulbena-Cabre, Carolina
Baez-Velasco, Silvia Rosado-Figuerola and Antonia Bulbena published as
a review article in the American Journal of Medical Genetics on November
9, 2021.
Statement
I am personally concerned about the aforementioned publication, because
firstly, it contains gross errors, and secondly, many parts of the publication
may be misinterpreted by doctors who have no knowledge of EDS. I am
writing this statement because I am very worried about the consequences
this paper can have for my patients. In the following paragraphs, I will
discuss some of the statements the authors made and provide arguments
on why I disagree.
EDS Symptoms Are Not Subjective
1. The authors state: “The psychiatric and psychological aspects of Ehlers-
Danlos Syndromes (EDS) have been neglected for many years. This
neglect is not only because of the significant stigma against mental illness
but also because of SUBJECTIVITY of many symptoms and the
misattributed psychological causality of them.”
EDS symptoms are not subjective. Nothing is more obvious than a
dislocated joint or heart rate readings in patients with dysautonomia. If
anything, the field of psychiatry is subjective.
The only symptom in EDS that may be subjective is pain, but the cause of
pain is apparent. Subluxing joints are visible to anyone who knows what to
look for, and so are flat feet and hyperextended joints. These are all painful
conditions.
Dysautonomia is not a subjective condition either. There are clear tests to
detect it: Tilt Table Test, QSART, and skin biopsy for small fiber peripheral
neuropathy.
Gastrointestinal issues like gastroparesis, intestinal dysmotility, acid reflux,
median arcuate ligament syndrome, Nutcracker syndrome and SMA
syndrome are actual conditions that can be detected with objective testing.
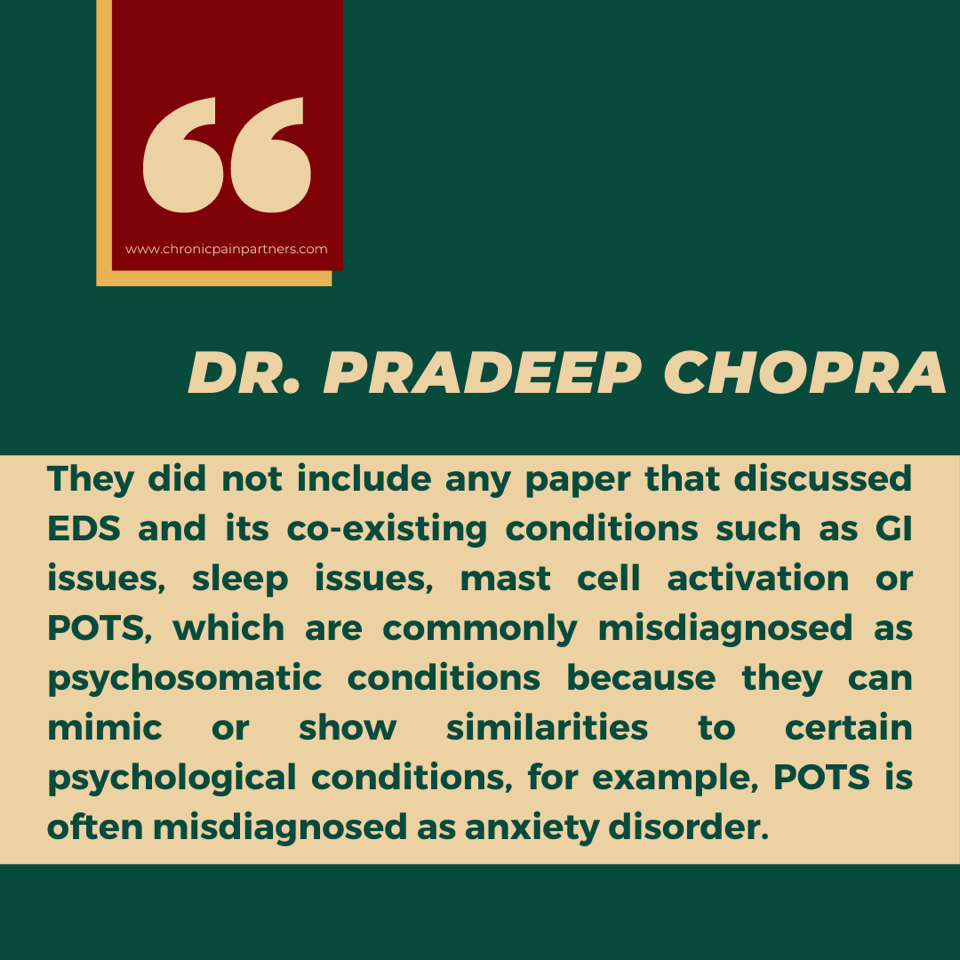
2. The authors did not include any papers about
comorbid conditions in their literature search.
For this paper, the authors did a literature search. They state: “The main
search terms used were ‘joint hypermobility syndrome,’ ‘Ehlers-Danlos,’
‘joint laxity,’ ‘anxiety,’ and each separate psychiatric diagnostic category.”
The authors only looked at papers that “…included if they reported any
psychiatric condition associated with joint hypermobility.” They did not
include any paper that discussed EDS and its co-existing conditions such
as GI issues, sleep issues, mast cell activation or POTS, which are
commonly misdiagnosed as psychosomatic conditions because they can
mimic or show similarities to certain psychological conditions. For example,
POTS is often misdiagnosed as an anxiety disorder.
3. The authors don‘t seem to understand the
bandwidth of EDS symptoms and how patients cope.
The authors write: “Another study by Baez-Velasco, Bulbena, Polanco-
Carrasco and Jaussaud (2019) found that several psychological and
cognitive factors affected pain chronicity and disability of hEDS. These
factors include cognitive problems and attention to body sensations,
negative emotions, and unhealthy patterns of activity.”
“Cognitive problems” are not psyche issues; POTS and MCAS cause brain
fog.
“Attention to body sensations”: this is true, but it’s not a mental issue. If my
hip keeps subluxing every time I stand up, I am going to pay attention to it.
After seeing over 800 patients with EDS, I have yet to find anyone with
negative emotions. People with EDS are some of the strongest and most
resilient people I know. I permanently have to insist that they tell me about
their pain. They are positive, cheerful, intelligent and hard-working people
who will push through everything to live their life.
“Unhealthy patterns of activity” does not make sense to me. Despite their
fatigue and pain, they push themselves every day to do more. They are
teachers, doctors, scientists, singers, actors, and some of the most
accomplished people despite their pain.
4. Patients with EDS are downplaying their pain; they
do not “catastrophize” it.
One paper the authors quoted, and which, in fact, is another publication by
one of the authors (Baeza-Velasco), claims: “Baeza-Velasco, Sinbaldi, and
Castori (2018) also studied low and high anxious people with hEDS and
found those with high anxious hEDS showed greater levels of pain
catastrophizing, somatosensory amplification (SSA) as well as poor social
functioning and general health.”
First, the source for the cited paper is incorrect. The source they listed is
about ADHD in EDS, with no mention of high or low anxiety or any of the
statements made.
Secondly, I want to talk about the wording:
“Pain Catastrophizing”: this is described in psyche literature as “a set of
exaggerated and negative cognitive and emotional schema brought to bear
during actual or anticipated painful stimulation [1].” This means that
patients with actual pain exaggerate how bad it is. Patients with EDS have
joint pain, muscle pain, headaches, spinal pain, abdominal pain, and
MCAS-related pain. They have more than enough reasons to always have
severe excruciating pain, and in my experience, they do not exaggerate
their pain. If anything, they usually play it down.
“Somatosensory amplification”: According to the literature, this is defined as
“the tendency to experience bodily sensations as intense, noxious or
disturbing and consisting of hypervigilance to bodily sensation, as well as a
predisposition to select out and concentrate on weak or infrequent
sensations and to react to sensations with emotions and thoughts that
intensify them [2].” What the authors are saying is that patients with EDS
are hypervigilant, and they purposely select small, infrequent issues and
make a big deal of them. Patients with EDS do not have SSA. There is no
data to support it. Patients with EDS are resilient to most issues. They are
definitely not hypervigilant or exaggerate small issues. They may worry
about becoming light-headed when upright (with dysautonomia), for
example, or about experiencing a dislocation if they walk, or reacting to
food when out at a restaurant (with MCAS). Everybody does. This is not
pathological.
“Poor social functioning and general health”: If someone constantly
experiences lax joints that sublux easily, a feeling of dizziness, heart racing,
nausea, stomach pain, the head feeling like it is going to explode from high
intracranial pressure and general body-wide pain than, of course, they are
avoiding going out into crowds. They are very active socially, for instance,
on social media, and always ready to help out each other. Despite all their
symptoms, they are functional and active to the best of their ability.
5. There is no accumulated evidence supporting
psych issues in EDS.
The authors state: “New research has confirmed that anxiety disorders are
very common in patients with EDS (Bulbena-Cabré & Bulbena, 2018).”
Looking at the article that they quoted here, there were some interesting
facts:
The paper that they are referring to was published yet again by the same
authors. It is a father and daughter team. This is a quote from the paper:
“Following the accumulated evidence on this topic over the past 30 years,
our group described the “Neuroconnective phenotype.” They did not
present any accumulated evidence. There was no data from 30 years.
The term ‘Neuroconnective phenotype’ means that patients with joint
hypermobility have psychopathologic features such as increased
interoception, exteroception, decreased proprioception, anticipatory
anxiety, phobias, mood symptoms, eating disorders, neurotic personality
traits, neurodevelopmental disorders, high sensitivity to loss and high
positive confrontation [3].
I am not sure what the “new research” is that they are referring to. It does
not seem to be from EDS patients.
6. Anxiety does not seem to be more common in EDS.
The authors say: “These findings are consistent with a study by our group
(Bulbena-Cabre et al., 2019) in which we found that children with JHS have
higher frequency of anxiety disorders and greater intensity of physiological
anxiety and somatic complaints and suggested that JHS might be used as
a marker for this anxiety phenotype in youngsters.”
This is a paper with the same family involved. Briefly, they went to a clinic
for children with mental health conditions. These kids already had anxiety
for whatever reason. They chose 160 (not randomized) and looked for how
many had hypermobility. To detect hypermobility, they used something
called the “Screening Questionnaire to detect Hypermobility (SQ-CH).” The
SQ-CH [4| was invented by one of the authors himself and is NOT an
officially recognized diagnostic tool. Out of 160 children with anxiety, only 13 had joint hypermobility using the SQ-CH criteria invented by one of the authors.
7. There is no evidence for eating disorders in patients with EDS.
The authors then go on to state that patients with EDS have eating
disorders. Eating disorder, as described by DSM IV, “is characterized by
severe disturbances in eating behavior.” It includes anorexia nervosa and
bulimia nervosa. Patients with EDS have often been misdiagnosed with the
above conditions mostly because they have stomach issues that went
undiagnosed. This is an incomplete list of gastrointestinal issues that
children and young adults with EDS go through: visceroptosis,
intussusception, median arcuate ligament syndrome, superior mesenteric
artery syndrome, gastroparesis, food intolerance, inflammatory bowel
disease. This list does not even include symptoms due to POTS and mast
cell activation syndrome. To diagnose someone with an “eating disorder,”
one has to rule out any other reason for gastrointestinal issues.
8. The paper is not a review article.
The paper is full of personal opinions. It does not fulfill the criteria for a
scientific review – with none or very weak data to back up their statements.
9. The paper may be used to harm patients.
And finally, my main concern: Unfortunately, this paper and other such
papers (there are some more) give child-abuse doctors a weapon against
young children and deprive older patients of good care.
References:
[1] Quartana PJ, Campbell CM, Edwards R. Pain Catastrophizing: a critical review. Expert Rev Neurother.
2009 May ; 9(5): 745–758. doi:10.1586/ERN.09.34.
[2] Abbey Susan E. Assessment of Patients with Somatization. Psychiatric Clinical Skill, 2006
[3] Bulbena Andrea, Bulbena Antonio. Anxiety and joint hypermobility: An unexpected association.
Current Psychiatry. Vol. 17, No.4
[4] Bulbena Antonio, Mallorqui-Bague et al. Self Reported questionnaire for the assessment of Joint
Hypemobility Syndrome (SQ-CH), a collagen condition, in Spanish Population. Eur. J.
Psychiat. vol.28 no.1 Zaragoza ene./mar. 2014 https://dx.doi.org/10.4321/S0213-61632014000100002
Written by Pradeep Chopra, MD, MHCM
Edited and fact-checked by Karina Sturm, Journalist





















Thank you for taking issue with this paper that subtly blames the victim I recently saw a post online about a patient with EB which is a genetic disease with a mutation in a collagen gene affecting skin causing open sores and ulcers all over the body. I couldn’t help but wonder if EDS had more visible manifestations like this if these types of conclusions about pain and coping would dare to be made.
Thank You Doctor Chopra!
Thank you for this very thorough rebuttal and reply.
Thank you Dr Chopra
Thank you thank you thank you.
We need a gatekeeper at the Gaslighting door. Thank you for stepping up to do so.
Does anyone else hear crackling, popping, clicking,,…in their skull. My cervical spine is shot. Can’t hold my head up without a brace. The cracking sound in my skull started a year after my degenerative cervical spine. The MRI found over ten conditions in my neck, even said brain matter was leaking into my cervical spine. Anyone else??
Thank you for believing us.
Thank you for this response.
Thank you for this! It is great to have someone countering this horrible “research” which has the potential to harm many.
I don’t know why some doctors are so fascinated with psychosomatic diagnoses that they keep trying to attach them to conditions which have actual physical, physiological, and neurological explanations.
Maybe we could push for a retraction of this paper based on all of its fictitious assertions?
Dear Mr Chopra.
My name is Mari Ángeles Díaz and I have a daughter with Ehlers Danlos Syndrome.
I have read your article carefully and I have to tell you that I disagree with you on several issues. You may be an extraordinary doctor who helps with pain, but I think you have understood very little of the articles you use in your discussion.
1. On point one, you will agree with me that for many years there has been a stigma towards mental health that unfortunately still continues. Regarding the subjectivity of the symptoms, the study highlights that a psychological cause is attributed to them when this is not really the case, and it does not refer to a dislocation (that is visible), or to dysautonomia (which fortunately is being diagnosed more and more). It refers to all the other problems that are definitely there and cause pain, discomfort, and disability, but don’t show up on tests most of the time.
2. When you do an article on pain, what do you look for to compare? Normally you look for other studies that already exist to compare what you are researching. In other words, if headaches are studied, they are not compared to foot pain… That is why it is normal that they have looked for other articles that have to do with psychology and psychiatry in order to carry out their discussion. That is what the scientific community does when it carries out a research article.
3. At no moment do the authors deny that there are POTS or MCAS. What seems incredible to me is that you reduce it to that and you do not consider the possibility that there could be other problems that cause cognitive deficit or disability, that is, you do not value anything more than the physical, leaving aside the mental aspect.
On the other hand, and here we fully agree, we all believe (the authors do too), that people who suffer from Ehlers-Danlos Syndrome are brave, strong, resilient and extremely courageous. I always recommend to those newly diagnosed with Ehlers-Danlos and hypermobility to watch a talk by Dr. Bulbena in which he talks about anxiety and hypermobility, but also about the enormous fighting capacity of those affected and EVERYONE is reflected in the doctor’s words.
Although they also suffer a lot and that is undoubtedly reflected in their spirit.
4. Can you tell me where you have read this? “What the authors are saying is that patients with EDS are hypervigilant and deliberately select small, infrequent problems and give them a lot of importance.” I am sorry to tell you that you have made a wrong interpretation. What I understand is that patients with EDS have a greater perception of their body, they are able to feel how their intestines move, listen to their own heart, the depth of their breathing and also, in many cases, they perceive what is around them. with greater intensity, however this is not considered to be a bad thing by the researchers, but simply something that happens. I think it’s good to be able to study it.
5. I have been able to read about the proposed neuroconnective phenotype. What I was able to extract is that it is a model that promotes the integration of all symptoms, both physical and psychological, to facilitate the diagnosis of EDS. In fact, all the symptoms/comorbidities are explained in the neuroconnective, and many of them are organic. Body and mind go together, and inevitably what happens to one affects the other, in whatever way, and both EDS and dysautonomia researchers strongly agree on that.
I could continue explaining my annoyance and concern for your article, since it ignores the mental part that is in each of us, but I think that is enough. I will only add two more things:
The first one is that, as you may know, between 80 and 90% of EDS patients are referred to a psychiatrist at some point in their lives, when doctors don’t know what’s going on and end up thinking it’s all in the patient’s head. That is why it is crucial that psychiatrists are trained in EDS, so they recognize the symptomatology (not only the psychiatric one), and, when suspected, they can refer the patient to receive the necessary care. There, Dr. Bulbena performs a crucial task: the classes that study with him know how to measure hypermobility and identify a case of EDS (this is very important) and he makes it known to his colleagues whenever he has the opportunity. A good psychiatrist is who knows how to see the organicity of symptoms, and we need more like him.
Dr. Bulbena accompanies his patients in the search for a diagnosis, which has to do with the physical, and at the same time seeks their mental wellness.
Last Thursday, May 26, I was able to attend a conference by Doctor Bulbena, in which there were at least 30 of his patients and they all agreed on how much Doctor Bulbena had helped them and that they were much better thanks to him.
I fully understand that when we hear the word “anxiety” we get scared, because it is what patients have been reduced to so many times, discrediting what was happening in their bodies. However, it is a symptom that is there, that many people with EDS suffer from and it can be the door to a much broader model.
The good thing about science, good science, is to question in order to advance, without labeling.
On a personal note, I will tell you that Dr. Bulbena treats my daughter and that he has traveled a journey with us (as he does with all his patients) without letting go our hand, in which he has treated her anxiety and depression, but he has also referred her to internists, digestives, neurosurgeons, neurologists, until we have found an adequate diagnosis and treatment.
He is a doctor who does not question, who validates your situation, and who knows EDS very well.
So please, do not judge great psychiatrists for the evil that others do (here I can tell you that there are many doctors from different specialties, who mistreat people with EDS due to ignorance), understand that these articles help people to comprehend the mental dimension of the EDS, and keep in mind that the professional background of Dr. Bulbena and his team is impeccable and that there are countless patients who certify it.
Whenever there is continuous and permanent pain, when patients are faced with misunderstanding, without a doubt, our mental part is affected.
Hopefully you can read the articles again under the point of view that I have offered you, eliminating prejudices. Body and mind go together and we must take care of them both.
Thanks for your attention.
Mari Angeles Diaz
If you wish to speak with Dr. Chopra, we recommend reaching out to him on his website: https://painri.com/