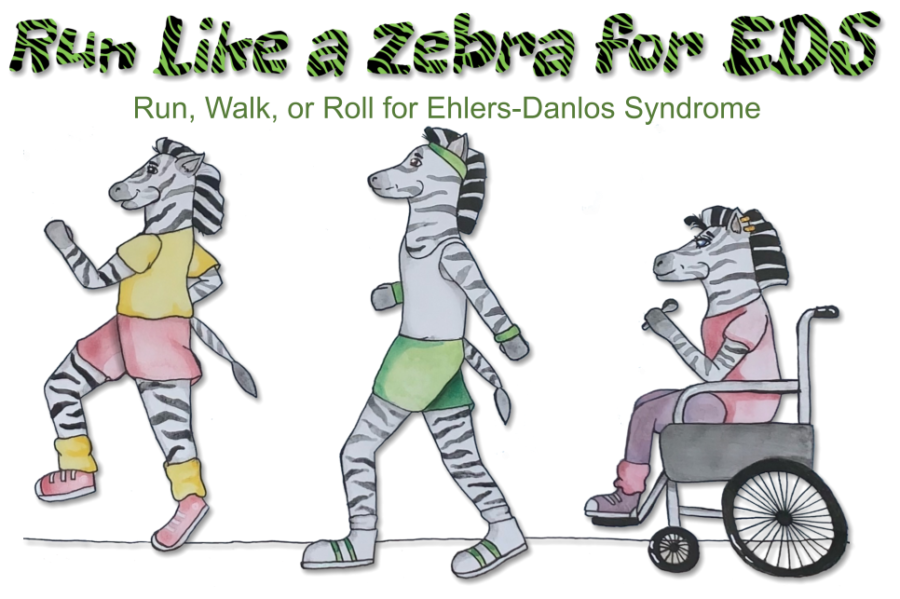
About EDS
Ehlers-Danlos Syndromes (EDS)
The Ehlers-Danlos Syndromes (EDS) are a group of diverse genetic and inherited connective tissue disorders that all cause a certain hypermobility of the joints, as well as fragile or soft skin. Since connective tissue is everywhere in the body, the EDS are multisystemic conditions, meaning depending on the type, EDS can cause symptoms in all organs and systems of the body and often leads to disability.
EDS was first described by Hippocrates in the year 400 B.C. when he noticed that there was a distinct group of people who presented with bruising and blood disorders. However, it gained part of its name in 1901 when Edvard Ehlers, a dermatologist from Denmark, described it as being a unique syndrome. In 1908 France, Henri-Alexandre Danlos noticed that fragile and hyperextensible skin should be a part of that syndrome [1] . Hence, Ehlers-Danlos Syndrome was officially born.
Most EDS types are considered rare and may affect an estimated 1 in 3,500 to <1 in 1,000,000 [2] individuals, based on which type (sometimes referred to as a “subtype”) an individual possesses. However, it has been proposed that the most common type, hypermobile EDS (hEDS) may affect as many as 1 in 500 and therefore is not rare, but rather rarely diagnosed [3] .
Connective tissue holds the body’s bones, muscles, organs, and other structures in place; hence, it is literally found everywhere in the human body. It is made up of two proteins: collagen and elastin [4]. Collagen is a fiber-like protein that is part of the body’s building blocks. It helps to make the body’s connective tissue strong, resilient, hydrated, and elastic, and it makes up 30% of the body’s total protein. It is found in the skin, bones, muscles, tendons, cartilage, and more. [5] Elastin is another protein, found in lungs, bladder, large blood vessels, ears’ cartilage, skin and ligaments. But, it is more of a stretchy fiber, like a rubber-band or hair “elastic” [6].
EDS is inherited in either an (a) autosomal dominant pattern or (b) an autosomal recessive pattern. An autosomal dominant pattern means that an individual has one copy of a mutated gene and one copy of a normal gene. So, this inheritance pattern needs just one parent to pass down the gene mutation [7]. An autosomal recessive pattern requires two mutated genes. Consequently, the biological parents must both have the genetic mutation and pass it down to the affected descendant [8]. Therefore, inheriting an autosomal recessive type of EDS is extraordinarily rare [9].
2017 International Diagnostic Criteria, Genetic Markers, Symptoms and Prevalence
As of 2017, there are 13 types of EDS, pursuant to research and discussion conducted by an international forum of EDS specialists from around the world [10]. The previous 1997 Villefranche Nosology [11] only categorized six main types with descriptive features (classical, vascular, hypermobile, arthrochalasis, kyphoscoliotic, and dermatosparaxis). The newer types include expanded forms of EDS and rarer forms that had been identified more recently, along with the major and minor diagnostic criteria, and the genetic markers responsible for each type.
EDS is usually diagnosed by a geneticist (or less often, a rheumatologist – depending on the country you live in) who has extensive knowledge about EDS, its types, symptoms, and diagnostic criteria. Doctors who wish to diagnose EDS must weigh both “major criteria” and “minor criteria” in assessing whether a patient has a particular form of EDS. In addition, there are genetic markers for all forms of EDS, except for Hypermobile EDS (hEDS) and certain Classical EDS (cEDS) patients. Therefore, other than hEDS most other suspected forms of EDS require molecular genetic testing to confirm accuracy.
This section focuses on information regarding the 13 types of EDS, the major and minor diagnostic criteria, genetic markers, prevalence, symptoms, and other useful information to help educate doctors, patients, loved ones, and others. This material, however, should not be used as a substitute for an official diagnosis by an experienced doctor.
More information on each type can be found below:
Classical EDS (cEDS)
ESTIMATED PREVALENCE: 1 per 10,000 to 1 per 20,000 [12]
INHERITANCE PATTERN: Autosomal Dominant
SYMPTOMS [13, 14]:
There is a large amount of symptom variance in Classical EDS (cEDS) patients. Some may be severely affected, while others lead an “almost-normal” life. cEDS mainly affects the skin, tissue, and organs. Skin hyperextensibility and atrophic scarring (depressed scars) must be present for cEDS to be diagnosed. Skin hyperextensibility is defined as stretching the skin beyond 1.5cm.
Other cEDS symptoms include easily bruised skin, poor wound healing, skin fragility (tearing skin), “cigarette paper” scars from cuts/surgeries, velvety soft skin, and highly and unusually flexible joints (hypermobility). Sometimes those with cEDS are born with hypotonia (weak muscle tone) and delayed motor development may occur.
DIAGNOSTIC CRITERIA [15]:
To diagnose cEDS, the following formula must be satisfied:
Major Criterion #1 + Major Criterion #2, OR Major Criterion 1 + three (3) Minor Criteria
A patient must have Major Criterion #1 (Skin hyperextensibility and atrophic scarring), plus have either Major Criterion #2 (Generalized joint hypermobility (GJH) or have three Minor Criteria. Most cases of cEDS can then be confirmed using molecular genetic testing. However, some patients may have cEDS without having a specific genetic marker. Also, other types and subtypes of EDS can have “crossover” attributes of cEDS. This means that, for example, in addition to having Hypermobile EDS, an individual may have attributes of cEDS, although these attributes are usually milder than those with cEDS.
The major and minor criteria and the genetic markers responsible for cEDS can be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers |
| 1. Skin hyperextensibility and atrophic scarring 2. Generalized joint hypermobility (GJH) | 1. Easy bruising 2. Soft, doughy skin 3. Skin fragility (or traumatic splitting) 4. Molluscoid pseudotumors 5. Subcutaneous spheroids 6. Hernia (or history thereof) 7. Epicanthal folds 8. Complications of joint hypermobility (e.g., sprains, luxation/subluxation, pain, flexible flatfoot) 9. Family history of a first-degree relative who meets clinical criteria | Major: COL5A1, COL5A2 Rare: COL1A1 |
Classical-like EDS (clEDS)
ESTIMATED PREVALENCE: <1 in 1,000,000 [16]
INHERITANCE PATTERN: Autosomal Recessive
SYMPTOMS:
Much like cEDS, clEDS is characterized by hypermobile joints, hyperextensible skin, easy bruising, and soft, velvety skin. However, it does not create atrophic scarring, as seen in cEDS. There are other features of clEDS that are not usually seen in cEDS, including foot and hand deformities, such as piezogenic papules, pes planus, broad forefeet, brachydactyly, and acrogeric (premature aging) of the skin of hands, and osteoporosis of the hips [17]. Symptoms may also include muscle weakness, myalgia (pain) and atrophy (wasting), hiatal hernia (protrusion of part of the stomach through the diaphragm in the chest cavity), high, narrow palate, scoliosis, hypotonia, and delayed motor skills. People with clEDS may experience severe fatigue, as well, due to hypermobility of joints and other complications.
DIAGNOSTIC CRITERIA [18]:
To diagnose clEDS, the following formula must be satisfied:
Major Criterion #1, #2, #3 + Positive Autosomal Recessive Family History
All three of the major criteria must be met, along with a positive family history that’s indicative of an inherited autosomal recessive pattern of transmission. Molecular genetic testing is then performed to confirm the diagnosis. clEDS is often referred to as the TNXB-related classical EDS because the genetic mutation responsible for this disorder is found in the TNXB gene.
The major and minor criteria and genetic markers responsible for clEDS can be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers |
| 1. Skin hyperextensibility, with velvety skin texture and absence of atrophic scarring 2. GJH with or without recurrent dislocations (most commonly shoulder and ankle) 3. Easily bruised skin/spontaneous ecchymoses | 1. Foot deformities: broad/plump forefoot, brachydactyly with excessive skin; pes planus; hallux valgus; piezogenic papules. 2. Edema in the legs in absence of cardiac failure 3. Mild proximal and distal muscle weakness 4. Axonal polyneuropathy 5. Atrophy of muscles in hands and feet 6. Acrogeric hands, mallet finger(s), clinodactyly, brachydactyly 7. Vaginal/uterus/rectal prolapse | TNXB |
Cardiac-Valvular EDS (cvEDS)
ESTIMATED PREVALENCE: <1 in 1,000,000 [19] (7 genetically-confirmed cases in the world, but fewer than 1,000 cases suspected)[20]
INHERITANCE PATTERN: Autosomal Recessive
SYMPTOMS:
Cardiac-Valvular EDS (cvEDS) often starts as a progressive disease of the mitral valve and may affect other cardiac valves. Patients may have joint hypermobility, hyperextensible skin, flatfeet, sagging of the lower eyelids (ptosis), and/or an absence of creases on one or more fingers.
DIAGNOSTIC CRITERIA [21]:
To diagnose cvEDS, the following formula must be satisfied:
Major Criterion #1 + Positive Autosomal Recessive Family History + One (1) Additional Major Criterion OR two (2) Minor Criteria
A patient must have Major Criterion #1 (severe, progressive cardiac valvular issues), a positive autosomal recessive type of family history, and one other Major Criterion, or two Minor Criteria. To confirm a suspected diagnosis, molecular genetic testing must be performed.
The major and minor criteria and the genetic markers responsible for cvEDS may be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers |
| 1. Severe progressive cardiac-valvular problems (aortic valve, mitral valve) 2. Skin involvement: skin hyperextensibility, atrophic scars, thin skin, easy bruising 3. Joint hypermobility (generalized or restricted to small joints) | 1. Inguinal hernia 2. Pectus deformity (especially excavatum) 3. Joint dislocations 4. Foot deformities: pes planus, pes planovalgus, hallux valgus | COL1A2 |
Vascular EDS (vEDS)
PREVALENCE: 1 in 50,000 to 200,000 [22]
INHERITANCE PATTERN: Autosomal Dominant (for this reason, genetic counseling is available, and often recommended, for couples who possess at least 1 copy of the mutated gene)
SYMPTOMS [23]:
Vascular EDS (vEDS) is mainly characterized by having fragile arteries, intestinal walls, and/or uterine walls. With vEDS, the arteries, organs, or intestines may perforate or rupture, due to the weakness of these structures. Other defining characteristics include thin, translucent (see-through) skin, prominent or unexplained bruising, protrusion of veins in the chest area, large eyes, a pinched or narrow nose, and thin lips (often the upper lip). Hypermobility of the joints is usually limited to the smaller joints of fingers and toes.
DIAGNOSTIC CRITERIA [24]:
To diagnose vEDS, the following formula must be satisfied:
Major Criterion #1, #2, #3 OR Minor Criterion #4 IF other Minor Criteria present
A patient must have Major Criterion #1 (family history of vEDS with a documented causative variant in COL3A1), Major Criterion #2 (Arterial rupture at a young age (under 40)), Major Criterion #3 (spontaneous sigmoid colon perforation in the absence of known diverticular disease or other bowel pathology), or Minor Criterion #4 (spontaneous pneumothorax) if other vEDS-consistent minor criteria are present. To confirm a suspected diagnosis, molecular genetic testing must be performed.
Most children with vEDS (about 60%) are diagnosed before they reach the age of 18 years, due to a positive family history. Half of the children tested for vEDS will experience a severe event, such as an arterial rupture, by the time they reach age 11 [25]. VEDS is considered one of the most severe forms of EDS because the life expectancy for those with vEDS is lower than average.
The major and minor criteria and genetic markers responsible for vEDS can be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers |
| 1. Family history of vEDS with a documented causative variant in COL3A1 2. Arterial rupture at a young age (under 40) 3. Spontaneous sigmoid colon perforation in the absence of known diverticular disease or other bowel pathology 4. Uterine rupture during the third trimester in the absence of previous C-section and/or severe peripartum perineum tears 5. Carotid-cavernous sinus fistula (CCSF) formation in the absence of trauma | 1. Bruising unrelated to identified trauma and/or in unusual sites such as cheeks and back 2. Thin, translucent skin with increased venous visibility 3. Characteristic facial appearance 4. Spontaneous pneumothorax 5. Acrogeria 6. Talipes equinovarus 7. Congenital hip dislocation 8. Hypermobility of small joints 9. Tendon and muscle rupture 10. Keratoconus 11. Gingival recession and gingival fragility 12. Early onset varicose veins (under age 30 and nulliparous if female) | Major: COL3A1 Rare: COL1A1 |
Hypermobile EDS (hEDS)
PREVALENCE: 1 in 3,500 to 1 in 5,000 [26] (but estimated 1:500, see above)
INHERITANCE PATTERN: Autosomal Dominant
SYMPTOMS [27, 28]:
Hypermobile EDS is the most common form of EDS. Measurable and/or observable symptoms [29] include hypermobile (very flexible) joints, frequent dislocations or subluxations of several joints, soft velvety skin, mildly stretchy skin, unexplained stretch marks, abdominal hernias, prolapse of the uterus, colon or pelvic floor (not due to other medical conditions) and atrophic scarring (collapsed, sometimes thin paper-like scars). Other observable symptoms may include blue sclera (whites of the eyes have a blue tint), having a high narrow palate, dental crowding, piezogenic papules on both feet (small, white circular protrusions near the bottom of heels when standing), slow motility, and heart manifestations like an enlarged aortic root or mitral valve prolapse.
However, some of the most debilitating symptoms of hEDS can be non-observable, subjective symptoms. This includes chronic widespread muscle and joint pain, nerve pain [30], severe headaches, migraines or “neck headaches”, fatigue (sometimes severe) [31], insomnia, and depression. Patients with hEDS also tend to have poor proprioception which, by itself, can add multiple injuries. There can also be crossover symptoms from another type of EDS. Many people must also deal with comorbid conditions, such as postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome (MCAS), Chiari I Malformation, immune/autoimmune issues, and many more [32].
hEDS and its criteria are evolving as research advances. Some of the possible mechanisms/causes behind hEDS that have been proposed in the past include mutations on MIA3 [33], which has been published in 2023, alongside research linking folate insufficiency, like the MTHFR genetic mutations, to hEDS [34]. Other earlier findings show a variant of LZST1, alterations in TPSAB1, mutations of Tenascin XB [35].
Several groups are studying the cause of hEDS as we write this. For instance, EDS Awareness has previously interviewed Dr. Russell “Chip” Norris of the Norris Lab at the Medical University of South Carolina, a lab dedicated to research on connective tissue diseases and abnormalities, including EDS. In 2018, Dr. Courtney Gensemer, then a first-year research student, was interested in studying hEDS due to her own experiences as a patient with hEDS. Her involvement transformed the lab into “one of the world’s largest groups studying hEDS.” In addition, the Ehlers-Danlos Society has enrolled a thousand people in its HEDGE study to expedite finding the cause of hEDS.
DIAGNOSTIC CRITERIA [36]:
Hypermobile EDS (hEDS) is the most in-depth and complex type of EDS to diagnose. This is because the symptoms and patient’s history are often extensive, and there are no definite genetic markers to confirm a suspected diagnosis. Prior to 2017, hEDS was diagnosed using the Beighton Score and/or the Brighton criteria. Now, the Beighton Score is just one component of the official criteria that must be satisfied. hEDS does not contain “major criteria” and “minor criteria” like other forms of EDS. Instead, it has a complex set of multifaceted tests that must be met, in their entirety.
There are now three (3) Major Criteria that must all be met to diagnose hEDS. Yet, within each criterion, there are additional features and tests which have their own objectives, symptom checklists, and assessments. It’s also important to note that there are many more symptoms than the ones listed under the diagnostic criteria. While they may constitute the official criteria, these symptoms can be measured objectively. There are many more objective and subjective symptoms than what is listed, so all criteria should be considered in the diagnostic process. Likewise, if a patient does not meet the hEDS criteria but is off by only one symptom or Beighton score, then a doctor must weigh the objective and subjective factors to make this determination.
The criteria for hEDS can be found in the chart and accompanying tables below. (A checklist can be downloaded here.)
| hEDS Major Diagnostic Criteria | Genetic Markers |
| ALL three (3) criteria must be met: 1. Features of Generalized Joint Hypermobility (GJH): A. Beighton Score of ≥6 for pre-pubertal children and adolescents B. Beighton Score of ≥5 for pubertal men & women up to 50 C. Beighton Score of ≥4 for men & women >50yo 2. Fulfillment of at least two of the following featured criteria (features A-C): A. Feature A – Systemic manifestations of a general connective tissue disorder (a total of five (5) must be present to satisfy Feature A) a. Unusually soft or velvety skin b. Mild skin hyperextensibility c. Unexplained striae such as striae distensae or rubrae at the back, groins, thighs, breasts, and/or abdomen in adolescents, men, or prepubertal women without a history of significant gain or loss of body fat or weight d. Bilateral piezogenic papules of the heel e. Recurrent or multiple abdominal hernia(s) (e.g., umbilical, inguinal, crural) f. Atrophic scarring involving at least two sites and without the formation of truly papyraceous and/or hemosideric scars as seen in classical EDS g. Pelvic floor, rectal, and/or uterine prolapse in children, men, or nulliparous women without a history of morbid obesity or other known predisposing medical condition h. Dental crowding and high or narrow palate i. Arachnodactyly, as defined in one or more of the following: (i) positive wrist sign (Steinberg sign) on both sides; (ii) positive thumb sign (Walker sign) on both sides j. Arm span-to-height ≥1.05 k. Mitral valve prolapse (MVP) mild or greater based on strict echocardiographic criteria l. Aortic root dilatation with Z-score > +2 B. Positive family history, with one or more first-degree relatives (biological mother, father, brother, sister) independently meeting the current diagnostic criteria for hEDS C. Musculoskeletal complications (must have at least one) a. Musculoskeletal pain in two or more limbs, recurring daily for at least 3 months b. Chronic, widespread pain for ≥3 months c. Recurrent joint dislocations or frank joint instability, in the absence of trauma: Three or more atraumatic dislocations in the same joint or two or more atraumatic dislocations in two different joints occurring at different times OR Medical confirmation of joint instability at two or more sites not related to trauma 3. ALL of the prerequisites must be met: a. Absence of unusual skin fragility, which should prompt consideration of other types of EDS b. Exclusion of other heritable and acquired connective tissue disorders, including autoimmune rheumatologic conditions. In patients with an acquired connective tissue disorder (e.g., lupus, rheumatoid arthritis, etc.), additional diagnosis of hEDS requires meeting both Features A and B of Criterion 2. Feature C of Criterion 2 (chronic pain and/or instability) cannot be counted towards a diagnosis of hEDS in this situation. c. Exclusion of alternative diagnoses that may also include joint hypermobility by means of hypotonia and/or connective tissue laxity. Alternative diagnoses and diagnostic categories include but are not limited to, neuromuscular disorders (e.g., myopathic EDS, Bethlem myopathy), other HCTD (e.g., other types of EDS, Loeys–Dietz syndrome, Marfan syndrome), and skeletal dysplasias (e.g., OI). Exclusion of these considerations may be based upon history, physical examination, and/or molecular genetic testing, as indicated. | Unknown |
The Beighton Score:
The Beighton Score is a simple clinical assessment used to evaluate joint hypermobility, particularly in the context of hypermobile Ehlers-Danlos syndrome (hEDS). It consists of a series of five tests, each assessing the flexibility of different joints. Each positive result is assigned one point, and a higher total score indicates greater joint hypermobility.
Here’s a step-by-step guide on how to perform the Beighton Score:
- Passive Dorsiflexion of Little Fingers:
- Ask the individual to extend their little finger backward as far as possible.
- If the finger can be passively bent backward more than 90 degrees, give one point.
- Passive Apposition of Thumbs to Forearm:
- Instruct the person to touch their thumb to the inside of their forearm.
- If the thumb can touch the forearm, give one point.
- Hyperextension of Elbows:
- Have the individual straighten their arms completely.
- If the elbows hyperextend beyond 10 degrees, give one point for each elbow.
- Hyperextension of Knees:
- Ask the person to stand and fully extend one leg at a time.
- If the knees hyperextend backward beyond 10 degrees, give one point for each knee.
- Forward Bending While Standing:
- Have the individual stand with their knees straight and bend forward to touch the ground with their palms.
- If the palms can touch the ground without bending the knees, give one point.
Add up the points from each of the five tests to determine the total Beighton Score. The maximum score is 9 points. A score of 5 or more is generally considered indicative of joint hypermobility.
It’s important to note that joint hypermobility can be present in various individuals, not only those with hEDS. The Beighton Score is just one component of a comprehensive assessment for hypermobility disorders, and a diagnosis should be made by a healthcare professional based on a thorough evaluation of the individual’s medical history, symptoms, and other clinical findings. Additionally, the Beighton Score only evaluates a few joints and therefore has been criticized for not being a good tool to evaluate joint hypermobility overall.
Arthrochalasia EDS (aEDS)
ESTIMATED PREVALENCE: <1 in 1,000,000 [39]
INHERITANCE PATTERN: Autosomal Dominant
SYMPTOMS [40, 41]:
Arthrochalasia EDS (aEDS) is most often found at birth, as severe dislocations of the smaller and larger joints can be either visually seen or reproduced upon manipulation. Almost all patients born with aEDS have bilateral hip dislocation. Many are also born with clubfoot, flatfoot, and/or skew foot (foot shaped like a “C”). It is common for other joints to sublux or dislocate, as well. Muscle weakness, skin hyperextensibility (stretchiness), easy bruising, and atrophic (cigar-like) scarring are routine.
Some patients with aEDS may also have mild craniofacial anomalies, called “dysmorphia of the face”, such as a large fontanelle (soft spot), blue sclera (blue in the whites of eyes), an unusually prominent forehead, or facial features which are undeveloped.
DIAGNOSTIC CRITERIA [42]:
To diagnose aEDS, the following formula must be satisfied:
Major Criterion #1 + Major Criterion #3, OR Major Criterion #2 + two (2) Minor Criteria
To be diagnosed, Major Criterion #1 (congenital bilateral hip dislocation), plus Major Criterion #3 (skin hyperextensibility), or Major Criterion #2 (severe generalized joint hypermobility, with many dislocations or subluxations), plus two Minor Criteria have to be satisfied. To confirm a suspected diagnosis, molecular genetic testing must be performed.
The major and minor criteria and the genetic markers responsible for aEDS can be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers |
| 1. Congenital bilateral hip dislocation 2. Severe GJH, with multiple dislocations/subluxations 3. Skin hyperextensibility | 1. Muscle hypotonia 2. Kyphoscoliosis 3. Radiologically mild osteopenia 4. Tissue fragility, including atrophic scars 5. Easily bruised skin | COL1A1 COL1A2 |
Dermatosparaxis EDS (dEDS)
ESTIMATED PREVALENCE: <1 in 1,000,000 [43]
INHERITANCE PATTERN: Autosomal Recessive
SYMPTOMS [44, 45]:
Dermatosparaxis EDS (dEDS) symptoms are present at birth or infancy and overwhelmingly involve the skin. Typically, symptoms involving the skin consist of soft, almost doughy-like skin that is often saggy, wrinkled or redundant, very fragile, and/or tears, bruises, and scars easily. Also, joint hypermobility, dysmorphic facial features (such as a large fontanelle, blue sclera, an unusually prominent forehead, or undeveloped facial features), and/or large hernias are often present. Premature rupture of membranes (PROM) (a tearing of the amniotic sac) can occur before birth.
Dermatosparaxis was first discovered in cattle and later found in sheep, cats, and dogs. The word “dermatosparaxis” means “tearing of the skin”. Thus, in animals, it results in large skin lacerations both at birth and early in life. These skin lacerations often result in infections and death at an early age. dEDS in humans is extremely rare, as it affects less than 1,000 in the USA.
DIAGNOSTIC CRITERIA [46]:
To diagnose dEDS, the following formula must be satisfied:
Major Criterion #1 + Major Criterion #2 + one other Major Criterion, OR three (3) Minor Criteria
To be diagnosed, Major Criterion #1 (extreme skin fragility with congenital or postnatal skin tears), plus Major Criterion #2 (craniofacial features, which are evident at birth, early infancy, or childhood), plus Major Criterion #3 (redundant, lax skin with excessive skin folds at the wrists and ankles), or three (3) Minor Criteria must be fulfilled. To confirm a suspected diagnosis, molecular genetic testing must be performed.
The major and minor criteria and the genetic markers responsible for dEDS can be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers |
| 1. Extreme skin fragility with congenital or postnatal skin tears 2. Characteristic craniofacial features, which are evident at birth or early infancy, or evolve later in childhood 3. Redundant, almost lax skin, with excessive skin folds at the wrists and ankles 4. Increased palmar wrinkling 5. Severe bruising with a risk of subcutaneous hematomas and hemorrhage 6. Umbilical hernia 7. Postnatal growth retardation 8. Short limbs, hand and feet 9. Perinatal complications due to connective tissue fragility | 1. Soft and doughy skin texture 2. Skin hyperextensibility 3. Atrophic scars 4. GJH 5. Complications of visceral fragility (e.g., bladder rupture, diaphragmatic rupture, rectal prolapse) 6. Delayed motor development 7. Osteopenia 8. Hirsutism 9. Tooth abnormalities 10. Refractive errors (myopia, astigmatism) 11. Strabismus | ADAMTS2 |
Kyphoscoliotic EDS (kEDS)
ESTIMATED PREVALENCE: <1 in 1,000,000 [47] (60 patients worldwide, as of June 9, 2022) [48]
INHERITANCE PATTERN: Autosomal Recessive
SYMPTOMS [49, 50]:
Kyphoscoliotic EDS (kEDS) symptoms consist of congenital muscle hypotonia and/or congenital, early onset of progressive/non-progressive kyphoscoliosis (forward rounding of the back that looks like slouching), osteopenia (low bone mass), osteoporosis (brittle, fragile bones), marfanoid structure and/or chest deformities. This can be accompanied by hyperextensible skin, skin that is fragile and easily bruises, atrophic (collapsed) scars, fragile sclera/oculus, hernias, rupture or aneurism of certain arteries, joint hypermobility, dysmorphic facial features (such as unusual positioning of eyes/ears or high palate) and additional features.
DIAGNOSTIC CRITERIA [51]:
To diagnose kEDS, the following formula must be satisfied:
Major Criterion #1 + Major Criterion #2 + Major Criterion #3, OR three (3) Minor Criteria
To diagnose kEDS, a patient must have Major Criterion #1 (congenital muscle hypotonia), plus Major Criterion #2 (congenital/early onset of kyphoscoliosis), plus Major Criterion #3 (general joint hypermobility, “GJH”) or three (3) Minor Criteria. Patients must also satisfy gene-specific criteria, according to the type of kEDS.
There are two main types of kEDS, sometimes called kEDS Type 1 and kEDS Type 2. These types are aligned with the mutated gene responsible for the specific type of kEDS a patient possesses, PLOD1 (Type 1) or FKBP14 (Type 2). Therefore, molecular genetic testing is required to confirm the diagnosis.
The major and minor criteria and the genetic markers responsible for kEDS can be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers |
| 1. Congenital muscle hypotonia 2. Congenital or early onset kyphoscoliosis (progressive or non-progressive) 3. GJH with dislocations/subluxations (shoulders, hips, and knees in particular) | 1. Skin hyperextensibility 2. Easily bruised skin 3. Rupture/aneurysm of a medium-sized artery 4. Osteopenia/osteoporosis 5. Blue sclerae 6. Hernia (umbilical or inguinal) 7. Pectus deformity 8. Marfanoid habitus 9. Talipes equinovarus 10. Refractive errors (myopia, hypermetropia) | PLOD1 FKBP14 |
Brittle Cornea Syndrome (BCS)
ESTIMATED PREVALENCE: <1 in 1,000,000 [52]
INHERITANCE PATTERN: Autosomal Recessive
SYMPTOMS:
Brittle Cornea Syndrome (BCS) affects the eyes, but can also involve the ears, joints, and skin. Characteristics of the eyes include thinning, fragility, protrusion, perforation and/or rupture of the cornea after no/minimal trauma, the presence of blue sclera, and nearsightedness. Patients may also present with deafness, skin and skeletal manifestations, due to mutations in the soft tissue.
DIAGNOSTIC CRITERIA [53]:
To diagnose BCS, the following formula must be satisfied:
Major Criterion #1 + one other Major Criterion, OR three (3) Minor Criteria
To diagnose BCS, a patient must have Major Criterion #1 (thin cornea, with or without rupture (central corneal thickness, often <400 µm), plus one other Major Criterion or three (3) Minor Criteria. Patients may also undergo molecular testing on two gene variants involved with respect to either ZNF469 or PRDM5. However, some patients possess neither gene variant, so genetic testing isn’t required for a diagnosis.
The major and minor criteria and the genetic markers responsible for BCS can be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers | ||
| 1. Thin cornea, with or without rupture (central corneal thickness often <400 µm) 2. Early-onset progressive keratoconus 3. Early-onset progressive keratoglobus 4. Blue sclerae | 1. Enucleation or corneal scarring as a result of previous rupture 2. Progressive loss of corneal stromal depth, especially in central cornea 3. High myopia, with normal or moderately increased axial length 4. Retinal detachment 5. Deafness, often with mixed conductive and sensorineural components, progressive, higher frequencies often more severely affected (“sloping” pure tone audiogram), 6. Hypercompliant tympanic membranes 7. Developmental dysplasia of the hip 8. Hypotonia in infancy, usually mild if present 9. Scoliosis 10. Arachnodactyly 11. Hypermobility of distal joints 12. Pes planus, hallux valgus 13. Mild contractures of fingers (especially 5th) 14. Soft, velvety skin, translucent skin | ZNF469 PRDM5 | ||
Spondylodysplastic EDS (spEDS)
ESTIMATED PREVALENCE: <1 in 1,000,000 [54]
INHERITANCE PATTERN: Autosomal Recessive
SYMPTOMS:
The symptoms unique to Spondylodysplastic EDS (spEDS) are short stature, muscle hypotonia (weak muscle tone), thin or scarce hair of the scalp and eyebrows (osteopenia), delayed motor development, and bowing of the arms and/or legs. However, spEDS also contains features that are central to other subtypes of EDS, including skin features, such as hyperextensibility, soft, almost doughy or translucent-looking skin, and abnormal scarring. Additionally, there may be small joint hypermobility and stretchy connective tissue.
DIAGNOSTIC CRITERIA [55]:
To diagnose spEDS, the following formula must be satisfied:
Major Criterion #1 + Major Criterion #2 + Radiographic Evidence + three (3) Minor Criteria
To diagnose spEDS, a patient must have Major Criterion #1 (short stature), plus Major Criterion #2 (congenital muscle hypotonia), plus radiographic evidence of musculoskeletal abnormalities, plus three (3) Minor Criteria (either gene-specific or in general). Ultimately, molecular testing is used to confirm the diagnosis.
The major and minor criteria and the genetic markers responsible for spEDS can be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers |
| 1. Short stature (progressive in childhood) 2. Muscle hypotonia (ranging from severe congenital, to mild later-onset) 3. Bowing of limbs | 1. Skin hyperextensibility, soft, doughy skin, thin translucent skin 2. Pes planus 3. Delayed motor development 4. Osteopenia 5. Delayed cognitive development | B4GALT7 B3GALT6 SLC39A13 |
Musculocontractural EDS (mcEDS)
ESTIMATED PREVALENCE: <1 in 1,000,000 [56]
INHERITANCE PATTERN: Autosomal Recessive
SYMPTOMS [57, 58]:
Musculocontractural EDS (mcEDS) is characterized by unique features usually present at birth or infancy, such as multiple contractures (tightness of muscles that shortens the joints), hypotonia (weak muscle tone), clubfoot, ear deformities, eye disorders, and/or craniofacial defects including large fontanelle (soft spot), blue sclera, high narrow palate, downward slanting or hypertelorism (increased space) of the palpebral fissures (space between the eyelids), or cleft palate. There may also be chest and spinal deformities, urogenital issues, diverticulitis (development of small bulging sacs) of the colon, pneumothorax (when a lung collapses due to air in the chest), abnormalities of the heart, kidneys, or intestines, mild cognitive impairment or delayed physical development.
mcEDS also contains features that are central to other subtypes of EDS, including hyperextensibility, soft, almost doughy or translucent-looking skin, and abnormal scarring. Additionally, there may be small joint hypermobility and stretchy connective tissue.
DIAGNOSTIC CRITERIA [59]:
To diagnose mcEDS, the formula depends on the age of the patient:
Birth/Early Childhood:
Major Criterion #1 + two of Major Criterion #2
To diagnose mcEDS at birth or in early childhood, a patient must have Major Criterion #1 (congenital multiple contractures), plus two of Major Criterion #2 (distinctive craniofacial features). Molecular testing must be used to confirm the diagnosis.
Adolescent/Adulthood:
Major Criterion #1 + three of Major Criterion #2
To diagnose mcEDS in adolescence or adulthood, a patient must have Major Criterion #1 (congenital multiple contractures), plus three of Major Criterion #2 (distinctive craniofacial features). Molecular testing must be used to confirm the diagnosis.
The major and minor criteria and the genetic markers responsible for mcEDS can be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers |
| 1. Congenital multiple contractures, characteristically adduction-flexion contractures and/or talipes equinovarus (clubfoot) 2. Characteristic craniofacial features, which are evident at birth or in early infancy 3. Characteristic cutaneous features including skin hyperextensibility, easy bruising, skin fragility with atrophic scars, increased palmar wrinkling | 1. Recurrent/chronic dislocations 2. Pectus deformities (flat, excavated) 3. Spinal deformities (scoliosis, kyphoscoliosis) 4. Peculiar fingers (tapering, slender, cylindrical) 5. Progressive talipes deformities (valgus, planus, cavum) 6. Large subcutaneous hematomas 7. Chronic constipation 8. Colonic diverticula 9. Pneumothorax/pneumohemothorax 10. Nephrolithiasis/cystolithiasis 11. Hydronephrosis 12. Cryptorchidism in males 13. Strabismus 14. Refractive errors (myopia, astigmatism) 15. Glaucoma/elevated intraocular pressure | CHST14 DSE |
Myophatic EDS (mEDS)
ESTIMATED PREVALENCE: <1 in 1,000,000 [60]
INHERITANCE PATTERN: Autosomal Recessive AND Autosomal Dominant (both found)
SYMPTOMS [61, 62]:
Myopathic EDS (mEDS) is usually characterized by myopathy (weakness) of the muscles and/or muscle hypotonia (poor muscle tone), that begins in childhood. There is often delayed motor development, as a result. Yet, in young adulthood, someone with mEDS often experiences a grace period, where these muscles become stronger until the patient’s forties, when they may become weak again. Often, patients with mEDS have large joint contractures (knees, hips, elbows, etc.), or shortening of the large joints/limbs due to tight muscles.
As with most forms of EDS, mEDS often presents with hypermobility (usually of the extremities), thick raised scarring, soft, doughy skin, and/or loose skin.
DIAGNOSTIC CRITERIA [63]:
To diagnose mEDS, the following formula must be satisfied, at the minimum:
Major Criterion #1 + one (1) other Major Criterion OR three (3) Minor Criteria
To diagnose mEDS, a patient must satisfy Major Criterion #1 (congenital muscle hypotonia, and/or muscle atrophy, which improves with age), plus one other Major Criterion or three (3) Minor Criteria. When diagnostic criteria are met, molecular testing is required to confirm a positive diagnosis.
The major and minor criteria and the genetic markers responsible for mEDS can be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers |
| 1. Congenital muscle hypotonia, and/or muscle atrophy, which improves with age 2. Proximal joint contractures (knee, hip, and elbow) 3. Hypermobility of distal joints | 1. Soft, doughy skin 2. Atrophic scarring 3. Motor developmental delay 4. Myopathy on muscle biopsy | COL12A1 |
Periodontal EDS (pEDS)
ESTIMATED PREVALENCE: <1 in 1,000,000 [64]
INHERITANCE PATTERN: Autosomal Dominant
SYMPTOMS [65]:
The main symptoms of Periodontal EDS (pEDS) are severe, intractable periodontitis and tooth recession in childhood or early teens, and/or a lack of attached gingiva. Periodontitis is a severe inflammation of the gums and other structures, which causes early tooth loss. While periodontitis is described in the population at large, including an increased number in those with EDS, with pEDS the tooth loss, gum recession, and inflammation are severe and occur in childhood or adolescence. Often, those with pEDS will have dentures or implants by the time they hit the age of 30.
Those with pEDS may also have discolored lower legs due to having fragile skin that easily tears, bruises, and scars, or due to pre-tibial discolorations (darkened lower legs). As with other forms of EDS, pEDS patients may also experience joint hypermobility, vascular issues, abnormal scarring, stretchy skin, and/or hernias.
DIAGNOSTIC CRITERIA [66]:
To diagnose pEDS, the following formula must be satisfied, at the minimum:
Major Criterion #1 OR Major Criterion #2 + two (2) other Major Criteria + one (1) Minor Criteria
In order to diagnose pEDS, a patient must have either Major Criterion #1 (early onset of severe, intractable periodontitis) or Major Criterion #2 (lack of attached gingiva), plus two (2) other Major Criteria and one (1) Minor Criterion. When diagnostic criteria are met, molecular testing is required to confirm a positive diagnosis.
Major and minor criteria and the genetic markers responsible for pEDS can be found in the chart below.
| Major Diagnostic Criteria | Minor Diagnostic Criteria | Genetic Markers |
| 1. Severe and intractable periodontitis of early onset (childhood or adolescence) 2. Lack of attached gingiva 3. Pretibial plaques 4. Family history of a first-degree relative who meets clinical criteria | 1. Easy bruising 2. Joint hypermobility, mostly distal joints 3. Skin hyperextensibility and fragility, abnormal scarring (wide or atrophic) 4. Increased rate of infections 5. Hernias 6. Marfanoid facial features 7. Acrogeria 8. Prominent vasculature | C1R C1S |
Sources
[1] Parapia, Liakat & Jackson, Carolyn. (2008). “Ehlers-Danlos syndrome – A historical review”, British Journal of Haematology. 141. 32-5. 10.1111/j.1365-2141.2008.06994.x.
[2] Orphanet, “Classical-like Ehlers-Danlos syndrome type 2“, Online: Orphanet. [Accessed April 12, 2023]
[3] Demmler, J.C., Atkinson, M.D., Reinhold, E.J., Choy, E., Lyons, R.A. and Brophy, S.T., 2019. Diagnosed prevalence of Ehlers-Danlos syndrome and hypermobility spectrum disorder in Wales, UK: a national electronic cohort study and case–control comparison. BMJ open, 9(11), p.e031365.
[4] Cleveland Clinic, “Ehlers Danlos Syndrome”, Online: https://my.clevelandclinic.org/health/diseases/17813-ehlers-danlos-syndrome, [Accessed June 16, 2023]
[5] Cleveland Clinic, “Collagen”, Online: Cleveland Clinic. [Accessed May 23, 2022]
[6] Cleveland Clinic, “Elastin”, Online: https://my.clevelandclinic.org/health/body/22482-elastin, [Accessed March 4, 2022]
[7] NIH, 2023. Autosomal dominant disorders. Online: https://www.genome.gov/genetics-glossary/Autosomal-Dominant-Disorder [Accessed November 10, 2023]
[8] NIH, 2023. Autosomal recessive disorders. Online: NIH. [Accessed November 10, 2023]
[9] Medline Plus, “Ehlers Danlos Syndrome”, https://medlineplus.gov/genetics/condition/ehlers-danlos-syndrome/#inheritance, [Accessed July 29, 2022]
[10] Malfait F, Francomano C, Byers P, et al., “The 2017 international classification of the Ehlers-Danlos syndromes.” Am J Med Genet C Semin Med Genet. 2017;175(1):8-26. doi:10.1002/ajmg.c.31552
[11] American Journal of Medical Genetics, 77:31±37 “Ehlers-Danlos Syndromes: Revised Nosology”, Villefranche, 1997
[12] Tyler Miklovic; Vanessa C. Sieg., “Ehlers Danlos Syndrome”, Online: https://www.ncbi.nlm.nih.gov/books/NBK549814/ [Accessed June 9, 2022]
[13] Nigel Burrows, “The Skin in Hypermobile Ehlers-Danlos Syndrome”, Online: https://www.ehlers-danlos.org/information/the-skin-in-hypermobile-ehlers-danlos-syndrome/ [Accessed Jan 4, 2016]
[14] Stembridge N, Doolan BJ, Lavallee ME, Hausser I, Pope FM, Seneviratne SL, Winship IM, Burrows NP. The role of cutaneous manifestations in the diagnosis of the Ehlers-Danlos syndromes. Skin Health Dis. 2022 Jul 15;3(1):e140. doi: 10.1002/ski2.140. PMID: 36751332; PMCID: PMC9892481.
[15] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[16] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[17] Orphanet, “Classical-like Ehlers-Danlos syndrome type 1“, Online: Orphanet. [Accessed November 10, 2023]
[18] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[19] The Ehlers Danlos Society, “What is EDS?”, Online: https://www.ehlers-danlos.com/what-is-eds/ [Accessed November 10, 2023]
[20] National Inst. of Health (NIH), “Cardiac-Valvular Ehlers-Danlos Syndrome”, Online: https://rarediseases.info.nih.gov/diseases/12613/cardiac-valvular-ehlers-danlos-syndrome [Accessed November 10, 2023]
[21] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[22] FightvEDS.org, “About Vascular Ehlers Danlos, The Basics of vEDS”, Online: FightvEDS [Accessed November 10, 2023]
[23] Byers PH. Vascular Ehlers-Danlos Syndrome. 1999 Sep 2 [Updated 2019 Feb 21]. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1494/
[24] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[25] Byers PH. “Vascular Ehlers-Danlos Syndrome”, 1999 Sep 2 [Updated 2019 Feb 21]. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1494/
[26] The Ehlers Danlos Society, “What is EDS?”, https://www.ehlers-danlos.com/what-is-eds/ [Accessed November 10, 2023]
[27] Levy HP. Hypermobile Ehlers-Danlos Syndrome. 2004 Oct 22 [Updated 2018 Jun 21]. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1279/
[28] Ehlers Danlos Support UK, “Hypermobile EDS & Hypermobile Spectrum Disorders”, Online: https://www.ehlers-danlos.org/what-is-eds/information-on-eds/hypermobile-eds-and-hypermobility-spectrum-disorders/ [Accessed November 10, 2023]
[29] Sturm, K., Jung, H. and Maier, A., 2022. Die Ehlers-Danlos-Syndrome. In Ratgeber Ehlers-Danlos-Syndrome: Komplexe Bindegewebserkrankungen einfach erklärt (pp. 1-39). Berlin, Heidelberg: Springer Berlin Heidelberg.
[30] Chopra, P., Tinkle, B., Hamonet, C., Brock, I., Gompel, A., Bulbena, A. and Francomano, C., 2017, March. Pain management in the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 212-219).
[31] Hakim, A., De Wandele, I., O’Callaghan, C., Pocinki, A. and Rowe, P., 2017, March. Chronic fatigue in Ehlers–Danlos syndrome—Hypermobile type. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 175-180).
[32] EDS News, “Other Conditions Common in EDS Patients”, Online: https://ehlersdanlosnews.com/health-insights/other-conditions-common-in-ehlers-danlos-syndrome-eds-patients/, [Accessed Dec 9, 2020]
[33] Junkiert-Czarnecka A, Pilarska-Deltow M, Bąk A, Heise M, Haus O. A novel mutation in collagen transport protein, MIA3 gene, detected in a patient with clinical symptoms of Ehlers–Danlos hypermobile syndrome [published online as ahead of print on January 5, 2023]. Adv Clin Exp Med. 2023. doi:10.17219/acem/158028
[34] Jacques Courseault, Catherine Kingry, Vivianne Morrison, Christiania Edstrom, Kelli Morrell, Lisa Jaubert, Victoria Elia, Gregory Bix, “Folate-dependent hypermobility syndrome: A proposed mechanism and diagnosis”, Heliyon, Volume 9, Issue 4, Apr 2023
[35] Lyons JJ, Yu X, Hughes JD, et al. Elevated basal serum tryptase identifies a multisystem disorder associated with increased TPSAB1 copy number. Nat Genet. 2016;48(12):1564-1569. doi:10.1038/ng.3696
[36] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[37] The Ehlers Danlos Society, “Assessing Joint Hypermobility”, Online: https://www.ehlers-danlos.com/assessing-joint-hypermobility/ [Accessed November 11, 2023]
[38] Malek, S., Reinhold, E.J. and Pearce, G.S., 2021. The Beighton Score as a measure of generalised joint hypermobility. Rheumatology International, 41(10), pp.1707-1716.
[39] The Ehlers Danlos Society, “What is EDS?”, Online: https://www.ehlers-danlos.com/what-is-eds/ [Accessed November 11, 2023]
[40] Klaassens M, Reinstein E, Hilhorst-Hofstee Y, Schrander JJ, Malfait F, Staal H, ten Have LC, Blaauw J, Roggeveen HC, Krakow D, De Paepe A, van Steensel MA, Pals G, Graham JM Jr, Schrander-Stumpel CT. Ehlers-Danlos Arthrochalasia type (VIIA-B)–expanding the phenotype: from prenatal life through adulthood. Clin Genet. 2012 Aug;82(2):121-30. doi: 10.1111/j.1399-0004.2011.01758.x. Epub 2011 Aug 24. PMID: 21801164; PMCID: PMC4026000.
[41] OMIM, “EHLERS-DANLOS SYNDROME, ARTHROCHALASIA TYPE, 1; EDSARTH1”, Online: https://www.omim.org/entry/130060, [Accessed December 15, 2020]
[42] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[43] The Ehlers Danlos Society, “What is EDS?”, Online: https://www.ehlers-danlos.com/what-is-eds/ [Accessed November 11, 2023]
[44] The Ehlers Danlos News, “Dermatosparaxis EDS”, https://ehlersdanlosnews.com/dermatosparaxis-eds/, [Accessed October 31, 2019]
[45] Geneskin, “Ehlers-Danlos Syndrome, Dermatosparaxis Type”, Online: https://geneskin.org/rare-genetic-diseases-of-the-skin/information-professionals/e-eo/ehlers-danlos-syndrome-dermatosparaxis-type [Accessed November 11, 2023]
[46] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[47] The Ehlers Danlos Society, “What is EDS?”, Online: https://www.ehlers-danlos.com/what-is-eds/ [Accessed November 11, 2023]
[48] Miklovic, T. and Sieg, V.C., 2019. Ehlers-Danlos syndrome.
[49] NIH/NCATS/GARD, 2023. “Kyphoscoliotic Ehlers-Danlos Syndrome”, Online: https://rarediseases.info.nih.gov/diseases/2083/kyphoscoliotic-ehlers-danlos-syndrome [Accessed November 11, 2023]
[50] Geneskin, “Ehlers-Danlos Syndrome, Kyphoscoliotic Type”, Online: https://geneskin.org/rare-genetic-diseases-of-the-skin/information-professionals/e-eo/ehlers-danlos-syndrome-kyphoscoliotic-type [Accessed November 11, 2023]
[51] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[52] The Ehlers Danlos Society, “What is EDS?”, Online: https://www.ehlers-danlos.com/what-is-eds/ [Accessed November 11, 2023]
[53] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[54] The Ehlers Danlos Society, “What is EDS?”, Online: https://www.ehlers-danlos.com/what-is-eds/ [Accessed November 11, 2023]
[55] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[56] The Ehlers Danlos Society, “What is EDS?”, Online: https://www.ehlers-danlos.com/what-is-eds/ [Accessed November 11, 2023]
[57] NIH/NCATS/GARD, “Musculocontractural Ehlers-Danlos Syndrome”, 2023. Online: https://rarediseases.info.nih.gov/diseases/8486/musculocontractural-ehlers-danlos-syndrome [Accessed November 11, 2023]
[58] Ehlers Danlos News, 2019. “Musculocontractural EDS”, Online: https://ehlersdanlosnews.com/musculocontractural-eds/ [Accessed November 11, 2023]
[59] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[60] The Ehlers Danlos Society, “What is EDS?”, Online: https://www.ehlers-danlos.com/what-is-eds/ [Accessed November 11, 2023]
[61] The Ehlers Danlos Society, “Myopathic Ehlers-Danlos Syndrome (mEDS)”, Online: https://www.ehlers-danlos.com/what-is-eds/myopathic-ehlers-danlos-syndrome-meds/ [Accessed November 11, 2023]
[62] Orphanet, 2023. “Myopathic EDS”, Online: https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=en&Expert=536516, [Accessed November 11, 2023]
[63] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
[64] The Ehlers Danlos Society, “What is EDS?”, Online: https://www.ehlers-danlos.com/what-is-eds/ [Accessed November 11, 2023]
[65] Kapferer-Seebacher I, van Dijk FS, Zschocke J. Periodontal Ehlers-Danlos Syndrome. 2021 Jul 29. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572429/
[66] Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., Bloom, L., Bowen, J.M., Brady, A.F., Burrows, N.P. and Castori, M., 2017, March. The 2017 international classification of the Ehlers–Danlos syndromes. In American Journal of Medical Genetics Part C: Seminars in Medical Genetics (Vol. 175, No. 1, pp. 8-26).
Last Updated: November 6, 2023
By Susan Jackson
About the author: Susan Jackson is a writer, editor and Ehlers-Danlos Syndrome (EDS) advocate who lives with her husband and nine-year-old daughter in south Florida. She’s been diagnosed with hypermobile EDS (hEDS), POTS, MCAS, Chiari I Malformation, AAI, CCI & multiple related issues. Susan enjoys spending quality time with her family, helping fellow EDSers find the care they need, exploring new healing modalities and working with crystals and reiki to heal her chronic pain.
DISCLAIMER – ChronicPainPartners.com/EDSawareness.com provides general information to the Ehlers Danlos Syndrome (EDS) community. Information on this website comes from a variety of sources that ChronicPainPartners.com/EDSawareness.com does not independently verify. Any views and/or opinions shared on ChronicPainPartners.com/EDSawareness.com should not be construed as medical advice. Always consult your doctor regarding your medical treatment or self-care.